UMMC Psychiatry marks 70 years of advancing mental health care in Mississippi

From its earliest days, psychiatry at the University of Mississippi Medical Center has asked not just how to treat illness, but also how to understand the human experience behind it. That question has guided the department for 70 years, shaping how physicians are trained, how care is delivered and how mental health is woven into the fabric of medicine across the state.
Today, the Department of Psychiatry and Human Behavior has become one of UMMC’s most diverse and far-reaching departments, with nationally recognized research programs, accredited training pathways, inpatient and outpatient services for all ages and statewide models designed to bring care to communities where it is needed most.
For current chair Dr. Mark Ladner, the roots of the department have grown intertwined with those of his family tree.
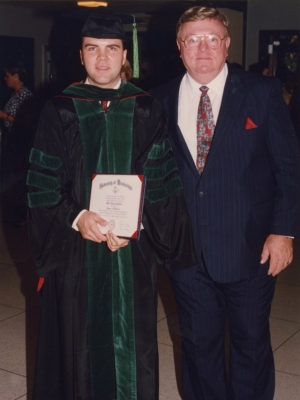
His father, Dr. George Dale Ladner, was among the first cohorts of medical students trained at UMMC, completing his degree in 1962. After serving in the U.S. Air Force for three years, he returned to UMMC in 1965 to complete his residency in psychiatry.
Just a couple decades later, his son would follow in his footsteps, attending medical school and psychiatry residency at UMMC and now in leadership of the very department his father helped build.

“It’s a unique privilege to chair the department where my father trained,” said Ladner. “There is something deeply meaningful about leading the same department that helped form my father as a physician and a psychiatrist. I did not envision this opportunity years ago. Serving as chair of the department connects my own leadership journey to the department’s history and long-standing commitment to quality training.
“Additionally, our family medical legacy continues as I have two daughters currently in the M1 class at UMMC. It is my upmost goal to reflect the same values my father showed me – professionalism and true concern for our patients and the field of medicine.”
The department was formally established in 1956, beginning with a single faculty member, one secretary and no dedicated inpatient beds. Early chairs relied heavily on partnerships with the Veterans Administration Hospital and Mississippi State Hospital at Whitfield to provide students and residents with clinical exposure.
Those early years required persistence. Proposals for an inpatient psychiatric unit at University Hospital were initially met with skepticism by state leaders, who questioned the need for specialized psychiatric care within an academic medical center.
But that skepticism gradually gave way to progress. By the early 1960s, UMMC opened its first inpatient psychiatric unit, marking a turning point for psychiatric education and care in Mississippi.
From the beginning, psychiatry at UMMC emphasized multidisciplinary care, integrating mental health into the broader medical curriculum and reinforcing the idea that psychiatric care belonged alongside other areas of care such as surgery, medicine and pediatrics.
By the 1970s and 1980s, UMMC Psychiatry had begun to distinguish itself nationally for its educational innovation.
A significant milestone was reached when faculty began using closed-circuit television and video recording to teach psychiatric interviewing skills, allowing students to observe real encounters without disrupting the session or patient-physician relationship. These efforts earned national attention and positioned UMMC as a leader in continuing psychiatric education at a time when few institutions were experimenting with audiovisual teaching tools.
Training at Mississippi State Hospital remained a defining component of the department. Medical students and residents gained immersive experience caring for patients with chronic and severe mental illness, learning that effective treatment extended well beyond hospitalization to include housing stability, family involvement and community reintegration.
The idea that the significance of psychiatry extends beyond medical treatment inside hospital walls would influence the department’s work for decades to come. As the department grew, so did its clinical scope.
In the 1980s and early 1990s, UMMC psychiatry faculty advanced emerging fields such as behavioral medicine, headache management, geriatric and child psychiatry, often ahead of broader national trends.
At the same time, the Sleep Disorders Center emerged as a regional and national leader. Under the direction of Dr. Howard Roffwarg, UMMC researchers conducted landmark studies on REM sleep, brain development and dreaming, contributing foundational knowledge to sleep medicine and influencing national classification standards.
By the mid-1980s, departmental growth required new infrastructure. Psychiatry expanded into additional clinical and office space across campus, renovated inpatient units and relocated child psychology services to accommodate growing faculty, research and training programs.
That growth set the stage for major research expansion in the decades that followed.
The Division of Neurobiology and Behavior Research brought basic scientists and clinicians together to study the biological foundations of mental illness. The division strengthened UMMC’s ability to translate discoveries from the laboratory to the bedside, supporting research into depression, schizophrenia, substance use disorders, neurodegenerative disease and suicide.
Its expansion was accelerated in 2002 with a landmark NIH Centers of Biomedical Research Excellence (COBRE) award, which created the Center for Psychiatric Neuroscience and positioned UMMC as a national hub for brain-based mental health research.
Research and clinical care also are bridged by the Center for Innovation and Discovery in Addictions (CIDA), which includes therapeutic discovery research as well as innovative telehealth treatment approaches. CIDA also includes UMMC's first outpatient addictions clinic, established in 2016.

“Having basic research in a clinical department gives us unique opportunities for synergy,” said Dr. James Rowlett, vice chair of neurobiology and behavior research. “For the scientists, we benefit from input received from clinicians treating those with the disorders we study. In turn, the clinicians can get input on their treatments from scientists at the forefront of state-of-the-art research in psychiatry.”
National recognition followed. In 2007, then-chair Dr. Grayson Norquist received the American Psychiatric Association’s Senior Scholar Award for advancing health services research. Norquist later assumed national leadership roles shaping mental health policy and outcomes research, including serving as chair of the Patient-Centered Outcomes Research Institute Board of Governors.
These efforts extended UMMC Psychiatry’s influence well beyond Mississippi, shaping how mental health outcomes, access and equity are measured nationwide.
As research and clinical programs expanded, the department focused on broadening access to mental health care across the state.
As psychiatry’s research and clinical footprint expanded, the department increasingly embedded its work within multidisciplinary centers designed to address complex conditions from multiple angles. Faculty play integral roles within UMMC’s Neuro Institute, collaborating across neurology, neurosurgery and rehabilitation to care for patients with disorders of the brain and nervous system.
Psychiatry is also a key partner in the MIND Center, which brings together specialists to diagnose and treat developmental and neurobehavioral conditions across the lifespan, and in the Center for the Advancement of Youth (CAY), which coordinates comprehensive behavioral and developmental care for children and families statewide. Through the ACT Center for Tobacco Treatment, psychiatry faculty have also helped advance evidence-based approaches to addiction treatment and smoking cessation, reinforcing the department’s long-standing focus on prevention and behavioral health integration.
These programs reflected a shift from centralized specialty care to systems-level solutions, addressing long-standing access gaps across Mississippi. Another critical component of that access-driven mission is the Child Access to Mental Health and Psychiatry Program (CHAMP), a statewide consultation and education service that supports primary care providers treating children with behavioral and emotional concerns.
Through CHAMP, UMMC psychiatrists and psychologists offer real-time guidance, training and referral support, helping clinicians manage conditions such as anxiety, depression, ADHD and trauma closer to home. The program, which is part of the Division of Psychology, reflects the department’s belief that strengthening the broader health care workforce is essential to improving mental health outcomes, particularly in rural and underserved communities.
“Programs like CHAMP allow us to extend psychiatric expertise far beyond our own clinics,” said Dr. Dustin Sarver, clinical director of the program. “By supporting primary care providers, we’re helping ensure children and families across Mississippi receive timely, informed mental health care, regardless of where they live.”
Today, the Department of Psychiatry and Human Behavior encompasses inpatient and outpatient services across the lifespan, accredited residency and fellowship programs, nationally recognized neuroscience research and expanding tele-mental health initiatives. Yet, its core identity remains consistent with the department that Dr. George Dale Ladner joined more than half a century ago.

“The department has a true tripartite mission involving clinical care, education and research, with significant contributions in all three areas,” said Dr. Scott Rodgers, associate vice chancellor for academic affairs and former chair of the department. “Though the department is relatively small in terms of faculty numbers, its footprint on our campus is large. Our clinical care programs are integral to the smooth functioning of the Adult and Children’s Hospitals.
“We are a core part of the educational program in the School of Medicine, and our residency programs attract superb candidates from across the nation, having become quite competitive in recent years. And our research programs have been truly top-notch, bringing in millions of research grant dollars and making discoveries that advance our understanding of illness and benefit all Mississippians. It is a department that I deeply respect and admire, and I am so grateful to Dr. [LouAnn] Woodward, [vice chancellor for health affairs] for allowing me to serve as its chair for 7.5 years.”
“This department has always been willing to adapt,” Ladner said. “But it has never lost sight of its purpose — to care for patients, to train physicians who understand the full human context of mental illness, and to develop psychiatrists for the state of Mississippi.”


