UMMC’s antimicrobial stewardship program receives national kudos
Since being recruited in 2011 to become the University of Mississippi Medical Center’s first medical director for antimicrobial stewardship, Dr. Jason Parham has championed antibiotic use driven by the right diagnosis, the right drug, the right dose, the right route and the right duration of treatment.
The hard work of Parham and his team is being recognized as among the best of the best on a national level. UMMC’s Antimicrobial Stewardship Program has been designated as a Center of Excellence by the Infectious Diseases Society of America. The society has recognized a total 64 institutions since 2018 as having that gold standard.
It validates Parham’s effort to change a hospital culture in which antibiotics, too often, are given inappropriately, from a provider prescribing a “Z-Pak” for a child’s sore throat to an inpatient being given a drug that’s stronger than necessary for longer than needed.

“It’s always nice to get external recognition from a panel of distinguished experts who have been doing stewardship for longer than we have,” said Parham, associate professor of infectious diseases in the Department of Medicine. It comes after a rigorous review of UMMC data and the society’s determination that “we’ve developed a comprehensive program that approaches antimicrobial stewardship in the right ways,” Parham said.
The Medical Center’s ASP, driven by ID physicians and ID-trained clinical pharmacists, strives to educate and persuade those who prescribe antibiotics to use them appropriately based on evidence and science. The frequent misuse of antibiotics has contributed to the growing problem of antibiotic resistance, a serious public health threat for those who are exposed to devastating antibiotic-resistant infections such as Methicillin-resistant Staphylococcus aureas, or MRSA.
The program “is one of the best in the country,” said UMMC Chief Medical Officer Dr. Michael Henderson. “Not only does it do the right thing for patients, but it is recognized by providers as bringing them up-to-date information on best practices in appropriate and safe use of antibiotics. In an increasingly complex field, UMMC is privileged to have such an invaluable resource.”
Much of the work of Parham and his staff has been behind the scenes, or via scrutiny of patients’ electronic medical records in search of opportunities to optimize their antibiotics. The team includes Dr. David Cretella and Dr. Mary Joyce Wingler, both clinical pharmacy specialists. If they see a need, the team discusses with a patient’s provider tweaks that best support evidence-based practices in prescribing.
They’ve made countless phone calls and had hundreds of in-person conversations with providers, working hand in hand with inpatient pharmacy, the Department of Pathology, the Department of Surgery, and the Department of Medicine’s Division of Infectious Diseases to standardize the proper use of antibiotics. They are collaborating with Pathology on the design and production of what’s known as antibiograms by tracking and gathering inpatient data on resistance trends and how susceptible local bacteria are to antibiotic resistance.
Changing a culture in which providers are sometimes too quick to inappropriately prescribe an antibiotic is a nationwide challenge and health care priority. The Centers for Disease Control and Prevention estimates that 20-50 percent of all antibiotics prescribed nationally in acute care hospitals are either unnecessary or inappropriate. The society reports an estimated 700,000 people in this country die annually due to antibiotic-resistant infections.
Parham’s team submitted “dozens of megabytes of data” to the society representing a review of the Medical Center’s ASP activities during 2018. “From the beginning, for us at UMMC, it’s always been about trying to improve the quality of patient care delivered, and as an extension of that, improving patient safety,” Parham said.
“We’ve tried to interact wherever antibiotics are being used, and to be at the table to be a part of those discussions,” Parham said. “We’re helping to gradually change the culture from one that viewed antibiotics as innocuous agents with no real risk to patients, to one that recognizes that the use of antibiotics sometimes has unintended consequences. We’ve tried to shift the culture from the idea that ‘there’s no harm in treating something with antibiotics for an extra few days,’ or ‘giving it for a virus just in case later it turns bacterial.’
“We counsel compliance with the best treatment guidelines available,” Parham said. “While every patient doesn’t fall into those guidelines, the vast majority should. We should deviate from them only for a good reason, and not overprescribe.”
The ASP team “has been a valuable tool for patient care on our service,” said Dr. Raman Palabindala, associate professor of medicine and director of the Division of Hospital Medicine. Palabindala is a hospitalist, a physician dedicated to the medical care of hospitalized patients.
“Not only is ASP a proper trigger to avoid unnecessary antibiotics, but it also acts as a great education tool,” Palabindala said. “The ASP staff is super knowledgeable and friendly in helping to take care of the orders. They are like ninjas - always keeping an eye on antibiotics and infections, and taking action when needed on time, and every time.”
The ASP is branching out to include the Medical Center’s departmental clinics, starting with the Department of Family Medicine. The goals, Parham said, include improving providers’ adherence to evidence-based antibiotic treatment for common infections – many of which are viral and don’t require antibiotics at all.
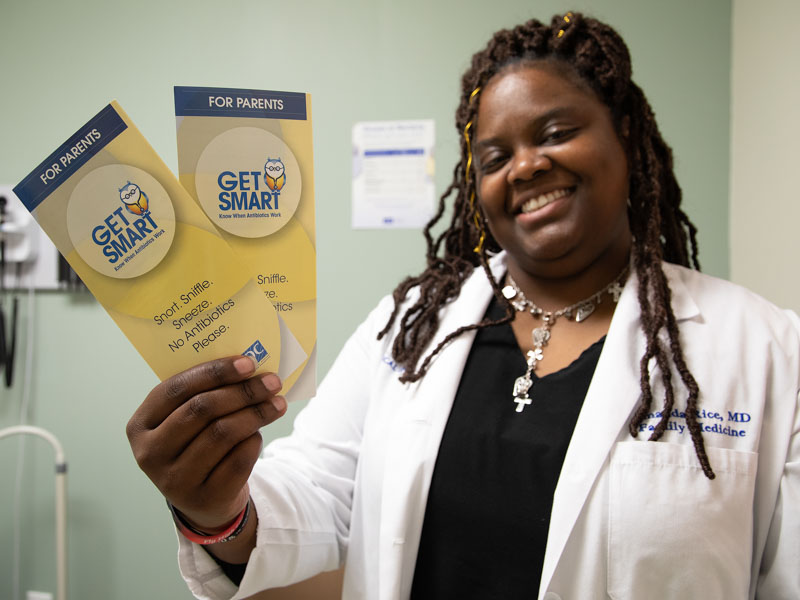
It’s not uncommon for patients to insist on an antibiotic, even though their illness doesn’t warrant one, said Dr. Amanda Rice, assistant professor of family medicine. “That’s why we (as caregivers) need to be educated on how to handle that,” she said.
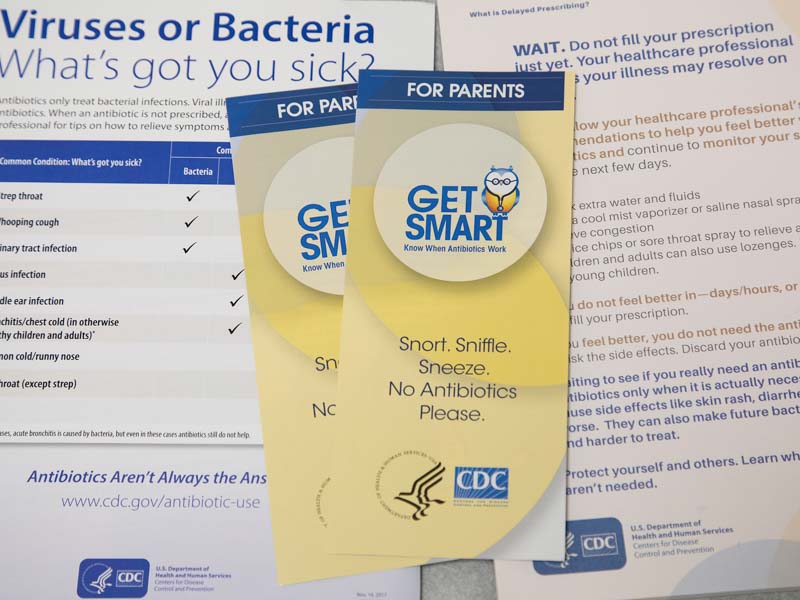
A new education program in Family Medicine aims to educate patients about when and why an antibiotic should be given, she said. Both patients and caregivers are receiving handouts that explain the difference between bacterial infections and viral infections. Information also is being posted on examination room walls “where patients will always see it,” Rice said.
“We are a teaching facility as well, and this gives us the chance to reach out to physicians,” she said. “We are keeping statistics on the amount of antibiotics that are being prescribed for a particular diagnosis.”
“We’re doing education with residents, their attending physicians and clinic staff, and we’ll be focusing on some areas where antibiotics are most commonly overprescribed, such as upper respiratory infections and bronchitis in otherwise healthy patients,” Parham said.
“The main area of focus so far has been in the adult wards and the ICU tower,” he said. “Once we felt the inpatient program had matured to the point to have the manpower to address outpatient prescribing, we thought it was time for us to make those big moves.”


