Study: healthy heart now, healthy brain later
Published in News Stories on April 20, 2017
A study published April 11 in the Journal of the American Medical Association found that people with two or more vascular disease risk factors during their 50s were three times more likely to have higher levels of amyloid plaque more than 20 years later.
This means your health at midlife could help determine your risk for Alzheimer's disease later on, said Dr. Tom Mosley, Hughes Chair and Director of the MIND Center at the University of Mississippi Medical Center and a co-author of the paper.
“There is a growing literature that suggests that what's good for the heart is also good for the brain,” he said.
Mosley leads the Jackson, Mississippi site of the Atherosclerosis Risk in Communities study. Since 1987, ARIC has tracked the cardiovascular health of thousands of participants in Jackson; Washington County, Maryland; Forsyth County, North Carolina; and Minneapolis, Minnesota.
As a prospective study, ARIC “is uniquely positioned to make a landmark contribution to our understanding of risk factors for dementia,” said Mosley, co-chair of the ARIC Neurocognitive study group.
This most recent study in JAMA examined data from 322 ARIC participants. They looked at five known cardiovascular disease risk factors: diabetes, obesity, high cholesterol, smoking and high blood pressure. Each contributes to atherosclerosis, the hardening and narrowing of arteries. As the leading direct cause of heart attack and stroke, atherosclerosis poses substantial health risks.
These five risk factors are tied to another condition: Alzheimer's disease.
“Prior work [has] found a robust relationship between cardiovascular risk factors and dementia and cognitive decline,” Mosley said. However, scientists have not identified a causal link, answering the question of what's changing inside the brain.
Scientists think amyloid plaques - misfolded proteins - damage neurons. This may lead to Alzheimer's, the most common form of dementia in the elderly.
For this study, researchers used positron emission tomography, or PET, to image amyloid in the study participants' brains 20 years after the initial ARIC exams. Nuclear medicine technologists intravenously administer a radioactive tracer called florbetapir. This attaches to the plaques in the brain. Through this uptake, the tracer helps visualize the plaques seen during PET scanning.
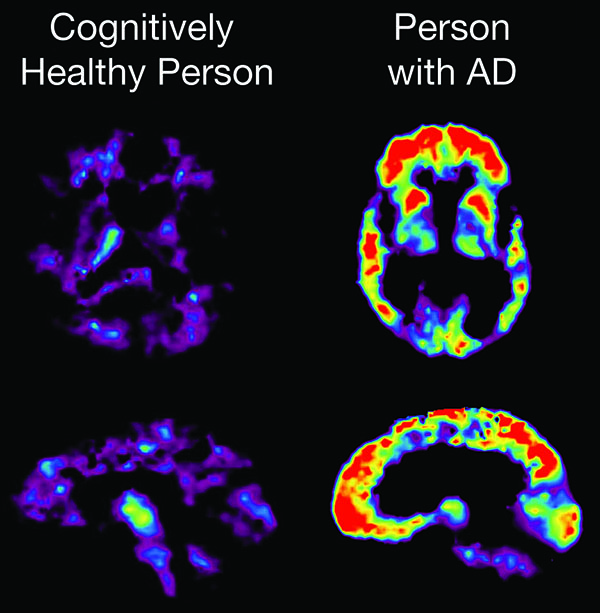
A PET scan reveals brain changes associated with Alzheimer's disease. At right, areas that glow red represent higher concentrations of amyloid plaque. (Image courtesy of the National Institute on Aging)
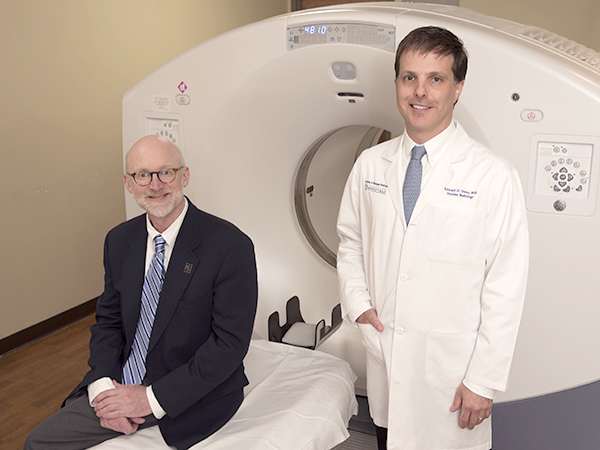
Dr. Edward Green, UMMC associate professor of radiology and study co-author, interprets clinical and research PET scans for the Jackson research participants.
“The areas of amyloid deposition on PET imaging basically 'light up' in comparison with normal areas of the brain where there is not any amyloid deposition,” Green said.
Green, Mosley and their co-authors found that obesity at the first ARIC exam doubled the likelihood of higher uptake. Further, they found that having any two or more of the five risk factors tripled the likelihood.
The findings suggests amyloid plaque deposition is “one potential mechanism of how cardiovascular risk factors may affect brain aging,” Mosley said.
The researchers note that the relatively small sample size may have affected their ability to detect certain relationships between vascular risk and amyloid. This might help account for some of the unexpected results.
“Previous findings in this study revealed that amyloid distribution differs by race,” Green said, but this most recent one did not. In addition, they didn't find a link between amyloid and a gene variant associated Alzheimer's disease. Another is that risk factors later in life weren't associated with the PET results.
“Either there's a vulnerable period - midlife or younger - or there's a cumulative effect over the decades.” Dr. Rebecca Gottesman, the lead study author and associate professor of neurology at Johns Hopkins University, told the New York Times. “Or it might be both.”
Because all five risk factors are largely preventable through diet, exercise and lifestyle choice, the results open an exciting possibility: the prevention of dementia.
“The link with cardiovascular risk factors is important because it suggests that brain changes may not be an inevitable part of aging, but may be caused by potentially modifiable factors,” Mosley said.
“While we wait for clinical trials to fully test the implications…there is little downside to putting these healthy habits in the practice now, and the sooner the better.”
Scientists and clinicians from the Mayo Clinic, Wake Forest University and Hagerstown Imaging in Maryland also contributed to the study. The work was supported by the National Heart, Lung, and Blood Institute, the National Institute of Neurological Disorders and Stroke, the National Institute on Aging and Avid Radiopharmaceuticals.


