The missing link: Research weighs obesity for dementia risks
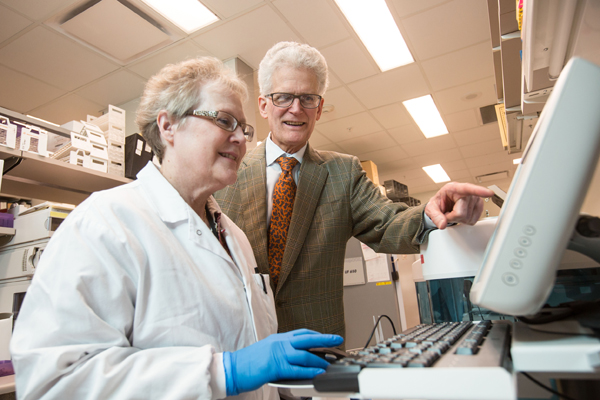
Two of the nation’s biggest health issues – obesity and dementia – are the target of the latest investigation to come from the University of Mississippi Medical Center. Specifically, Dr. Gwen Windham is looking for evidence of obesity as a potential risk factor for developing dementia later in life.
Windham, associate professor of clinical geriatrics/gerontology at UMMC and director of the MIND Center Clinic, has been awarded a $1.2 million grant from the National Institute on Aging, part of the National Institutes of Health, to look into a potential causal relationship between the two factors.

Windham said focusing on modifiable risk factors – in this case, obesity – and understanding how changing that factor can reduce the risk of dementia is the goal of her study.
Leading the study from Jackson, Windham is working with researchers at Mayo Clinic and Boston University to examine previously collected samples from study volunteers at UMMC.
The other two medical centers are responsible for analyzing the blood samples and providing expertise on the biomarkers of interest, said Windham. Those samples were collected during a previous years-long UMMC study measuring the effects of hypertension on the brain.
Dr. Stephen Turner, a nephrology and hypertension researcher at Mayo Clinic, was involved in the former study involving UMMC and now works with Windham on her new study.
Turner said the MIND Center, UMMC’s Alzheimer’s and dementia research and clinical care initiative, and its director, Dr. Tom Mosley, had the foresight in the former study – which ran in the mid- to late-2000s – to ask researchers to determine the cognitive function of participants.
By adding those extra measurements in an earlier study with already vetted participants, Mosley and others created an information pool from which later studies could pull.
“It just doesn’t make sense to ignore all you did before and start a new study,” said Turner.
Windham said by using the blood samples, biological measurements and cognitive tests gathered from the earlier study actually saves time and money, an increasingly difficult commodity to acquire for new studies.
“We're very proud of her,” said Mosley, a colleague and mentor of Windham. “Getting funding from the National Institutes of Health is highly competitive and always a challenge. She wrote a fantastic grant, got a good score and got it funded.”
Mosley said Windham’s study is another example of UMMC’s collaborative efforts with Mayo Clinic, and also holds powerful implications for a region where obesity remains a widespread problem.
“It's very relevant for Mississippi,” he said of Windham’s study. “We have a lot of obesity. How does that relate to an aging brain? It's a very relevant question for us.”
Windham said certain population groups seem to be at an increased risk of obesity and dementia. The Jackson study is comprised solely of African-American participants, one such group considered to be at a higher risk for both conditions.
“We do think that there's pretty good evidence that cardiovascular risk factors – like diabetes and hypertension – increase the risk of dementia,” she said. “And we've shown that it does affect cognitive decline over time just looking at even mid-life hypertension and diabetes.
“Then you follow people for 20 years, and you see those with these conditions develop more cognitive decline that those who don't,” Windham added. “So this is a good site to investigate the relationships of obesity as well as cardiovascular risk factors on outcomes including dementia and cognitive decline.”


