Psychiatry program harbors homeless, uninsured

Published in News Stories on October 27, 2016
Since mid-summer, demand has tripled for a new mental health program offered at no charge to those who have no insurance or have no home.
When the Psychiatry Outreach Program (POP) opened its doors on July 23, three or four people showed up at the Jackson Free Clinic on a Saturday afternoon complaining of depression, anxiety, insomnia or some other concern that might have remained untreated.
Three months later, on October 15, the number was 11; that's how many homeless or uninsured Jackson-area residents had signed up for appointments with the staff of volunteers led by attending physician Dr. Chasity Torrence, assistant professor of psychiatry in the Department of Psychiatry and Human Behavior.
“They're fighting for a place to be seen,” she said.
It's because of this struggle - magnified by the state's recent cuts to mental health programs - that Torrence developed POP with psychiatry residents Dr. Charles Richardson and Dr. Matthew Walker.
The thrust of POP was inspired by a presentation Torrence and others witnessed in the spring from Dr. Sheryl Fleisch, assistant professor at Vanderbilt University and medical director of a psychiatry program she and her team take to the streets of Nashville.
Eventually, that's what POP's volunteers would like to do: “We want to go to the patients, not make them all come to the clinic,” said Richardson, a fourth-year resident.
“Maybe one day a week we could offer 'street psychiatry' - that's kind of the working name.”
For now, patients make appointments at the student-run Jackson Free Clinic next to the Humble Church of God in Christ on Martin Luther King Jr. Drive in west Jackson; begun more than 15 years ago, the clinic, with its staff of medical students supervised by physicians, provides free, non-emergency care to adults, ages 18 to 65, who can't pay.

Dr. Chasity Torrence, right, and fourth-year medical student Jonathan Baker review a case on October 15 at the Jackson Free Clinic.
Since July, the clinic's volunteers have been working with the staff of POP to sponsor “mental health day,” reserving two exam rooms for the new psychiatry program, whose volunteers also include Dr. Jon Jackson, assistant professor of psychiatry, and fourth-year medical students Jonathan Baker and Yolonda Ross.
Most people seeking mental health services from POP are referrals from the regular medical staff of the Jackson Free Clinic, which is open every Saturday; in contrast, and for now at least, POP is available only on the third Saturday of each month, from around noon until 4 p.m.
With those limited hours, coupled with growing demand, POP's staff is seeking to work with other free programs, such as Mission First and We Will Go Ministries to help even more people.
At stake is the well-being and quality of life, not only for the homeless, but also for Jackson-area residents like Linda Poarch of Flora.
“I'm ready to get off this walker and on with my life,” said Poarch, one of the patients who showed up on October 15. She is suffering from insomnia and a depressed mood linked to pain that wracks her left side and back, and from her leg from the knee down, she said.
“I can't afford insurance,” she said. “I wouldn't be able to go anywhere else except the emergency room. They've helped me a lot here.”
Two days after Poarch visited the clinic, researchers at a Las Vegas conference reported that patients who bring their mental health issues to the emergency room are more likely to be uninsured, compared to other patients.
Presented at the annual meeting of the American College of Emergency Physicians, the researchers' report also noted that emergency psychiatric patients, compared with patients with physical problems: rely more on the ER for treatment; are more often admitted to the hospital from the ER; are kept in the ER longer; and, because of weaknesses in the mental health care system, cannot be sent home after just one or two days.
This all adds up to greater costs for health care - for everyone. As for homeless patients, emergency departments are not prepared to handle their mental health needs. At UMMC, a homeless person spends about three nights per visit in the hospital, costing up to $9,000.
“If the patients could come meet us here at the free clinic, we could ease the burden on emergency rooms and the clinics,” said Torrence, who is also a staff psychiatrist at Mississippi State Hospital.
“So we hope to show, eventually, that this can affect the bottom line.”
While the state's homeless population dropped by 11 percent in 2015, as reported by the National Alliance to End Homelessness, it is still around 2,000, with one-third of those living in Jackson.
Homelessness spreads when, along with other factors, there is a lack of affordable housing, substance abuse services, good-paying jobs and mental health services. This year, after legislators cut the state's mental health budget by $8.3 million, the result was a reduction in the number of beds serving psychiatric patients and the shutdown of a chemical dependency program.
When psychiatric patients show up at UMMC's ER, many have been kicked out of group homes and are looking for shelter, Torrence said. Many don't have their medications, which can lead to illegal drug use.
“Among all homeless people, two-thirds have a drug addiction, and one-third have a mental illness,” she said.
While some patients turn to local mental health centers for help, they are charged on a sliding pay scale. All of POP's services are free. Patients must cover their own prescription drug costs, but, even then, the staff will do online searches of retail pharmacies to find the lowest prices.
For $4 a month, for instance, Poarch is able to get medication that will treat her insomnia, depression and pain, Richardson said.
Despite the growing caseload, the staff hopes to expand the scope of POP, making it part of the psychiatry residency program and using it to strengthen the department's presence for the community's mental health patients who are not being served.
“They have such a need,” said Torrence, who calls them “the forgotten.”

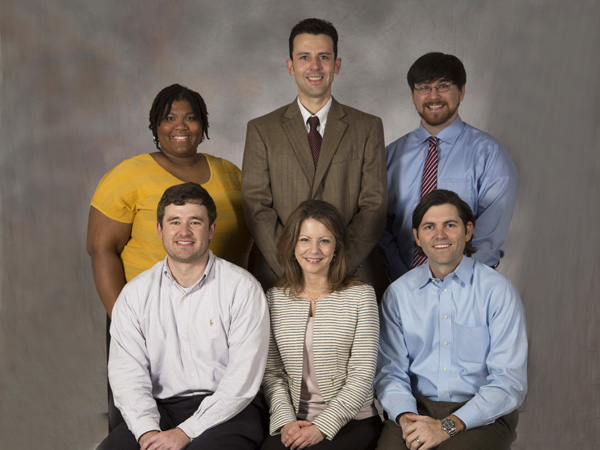
Staff members of the Psychiatry Outreach Program are, front row, from left, row, co-founders Dr. Matthew Walker, a third-year resident; Dr. Chasity Torrence, assistant professor of psychiatry; and fourth-year resident Dr. Charles "Chaz" Richardson; back row, from left, volunteers Yolonda Ross, a fourth-year medical student; Dr. Jon Jackson, assistant professor of psychiatry; and Jonathan Baker, a fourth-year medical student.
For more information about the Psychiatry Outreach Program and the Jackson Free Clinic, go to www.jacksonfreeclinic.org, or call 601-350-5161.
Photos
 | PGA-Sanderson-Video-Shoot_14.jpg High Resolution Medium Resolution Low Resolution |
 | PGA-Sanderson-Video-Shoot_27.jpg High Resolution Medium Resolution Low Resolution |
 | 03PGA-Sanderson-Video-Shoot_22.jpg High Resolution Medium Resolution Low Resolution |


