Researcher’s goal: Find the best chemo for each patient
A cancer researcher's most recent discovery ultimately may enable doctors to identify the drug or drug combination that works best against glioblastoma, a type of brain cancer, before treatment begins.
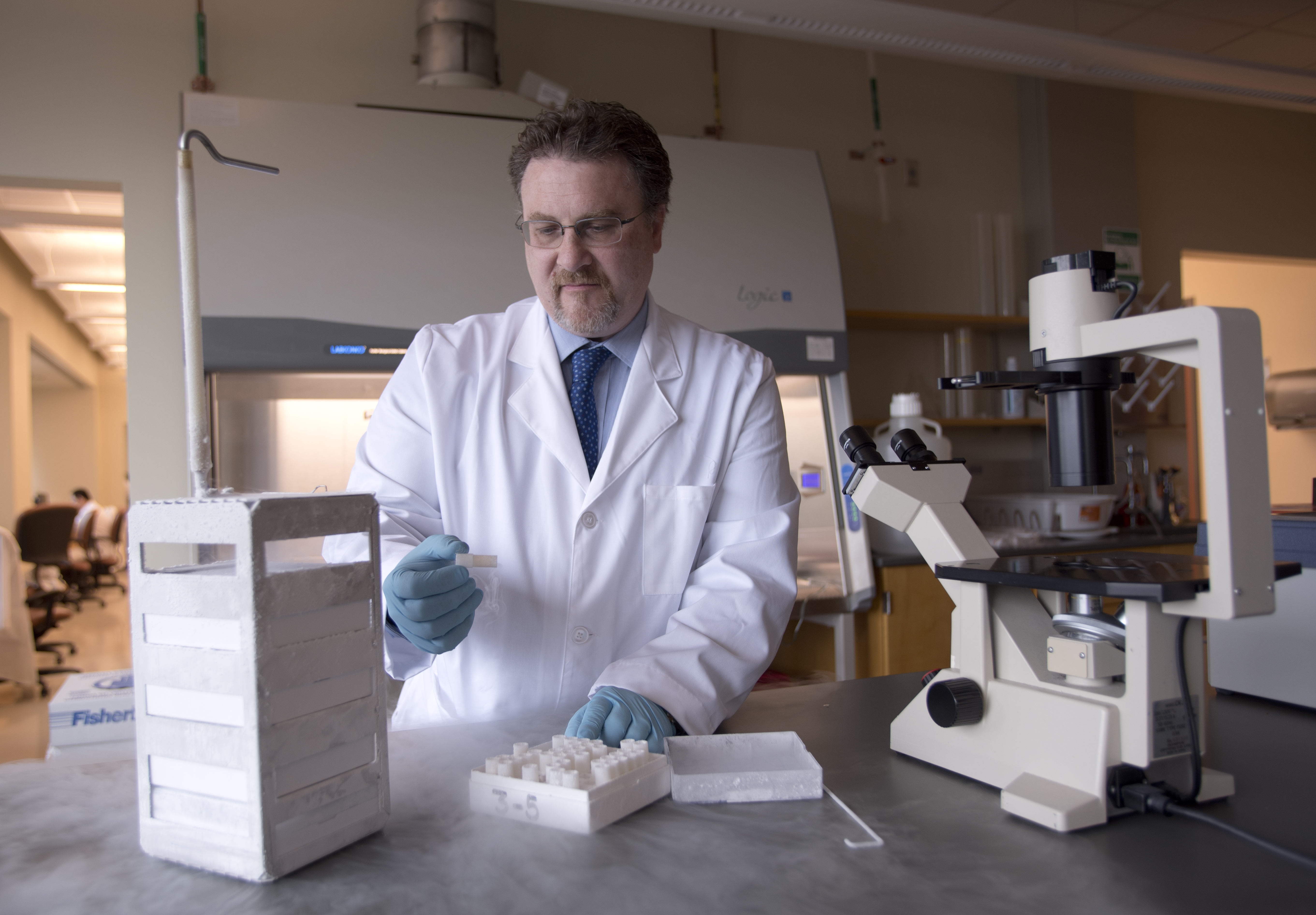
Dr. Pier Paolo Claudio, who holds appointments at the University of Mississippi Medical Center's Cancer Institute and at the University of Mississippi, worked with a team to ascertain whether tumors taken from cancer patients and tested in the laboratory could predict responses.
Study results show the process they used to test bulk tumor cells and cancer stem cells in the lab correlates with progress patients showed or didn't show with current recommended therapies. The next step will be testing the process in clinical trials.
Tumor cells treated with drugs that acted on both bulk tumor cells and cancer stem cells showed the best response. Those treated with drugs that had little effect on one or the other saw an earlier recurrence of the cancer.
Patients who had more than 40 percent of their cancer stem cells killed by temozolomide in the assay had longer times before tumor recurrence than those whose had fewer cells killed in the assay.
“We'll need further clinical trials but results of this study bring us closer to offering personalized therapy for this type of brain cancer,” Claudio said.

"Across all of cancer chemotherapy we have been bedeviled by the development of resistance to therapy,” said Dr. John Ruckdeschel, Cancer Institute director. “While long thought to be related to clones of cancer cells within a tumor that were selected out because they could resist the therapy, more recent theories have suggested that self-replicating stem cells could be the culprits.
“Dr. Claudio and his colleagues have developed an exciting assay that allows study of both stem cells and non-stem cells (bulk) and shows that differential responses in these cell compartments can predict clinical benefit, or lack thereof,” Ruckdeschel said. “We are very excited to be working toward confirmatory clinical trials.”
Some results were especially exciting: when drugs worked against both the tumor's cancer stem cells and bulk cells the cancer recurred much later than when the cancer stem cells were unaffected by therapy.
Glioblastomas most commonly affect older men, representing about 15 percent of all primary brain tumors. Currently, there is no cure. The current standard of care consists of surgery to remove as much of the tumor as possible, followed by use of the chemotherapy drug temozolomide and radiation therapy.
In a paper published online Feb. 13 in the journal Translational Oncology, Claudio, professor of biomolecular sciences, and his team outline the study process. Authors are from UMMC, the University of Mississippi, Marshall University and the University of Salerno in Italy.
Researchers know some glioblastoma patients respond to current therapies but others do not and that glioblastoma tumors have a small number of cancer stem cells that seem to help the tumor grow, resist treatment, maintain its presence in the brain and make the cancer recur.
Claudio and his team used ChemoID, a second generation drug sensitivity assay, to test 13 chemotherapy drugs and two combination chemotherapies approved for glioblastoma against tumors from each patient, highlighting which drugs might work best.
In some cases they found one drug worked best against bulk tumor cells and another worked better against the cancer stem cells.
Previous studies that looked at how effective drugs were against bulk cancer cells, did not specifically test the drugs on cancer stem cells. Some studies also used higher or lower dosages than recommended for patients. Claudio said this team sought to replicate the amount of drug given a patient and the time it could affect the tumor.
“The major problem with GBM treatment is that several of the different clinically-acceptable and equivalent treatment choices are identified in current treatment guidelines with insufficient evidence to indicate that any one agent is superior to any other,” the authors said in the paper.
Working with 42 patients, 41 recently diagnosed and one with a recurrent tumor, Claudio and his team tested tumors cells removed against the ChemoID assay.
In each case, doctors and patients chose the current standard of care: surgery to remove as much tumor as possible followed by temozolomide and radiation therapy. Claudio and his team compared the results of the assays on the tumors to the progress of each patient.
“We found those patients with no benefit from temozolomide could have benefited from another drug,” Claudio said.
In the study, ChemoID indicated a drug or combination “potentially more optimal” than temozolomide could have been used for 34 of the 41 patients based on cancer stem cell testing and 27 of 41 patients based on bulk tumor cell testing.
Although there's more work to complete, Dr. Mark Anderson, assistant professor of neurology and a member of the Cancer Institute's brain cancer program, said the study is encouraging.

“Intervention with alternate treatment earlier in therapy could help find a more effective therapy before further progression of disease, which increases the chance of a better outcome,” he said.
In practical terms, it takes about 21 days to complete the ChemoID assay once researchers receive a live biopsy. Patients need about that long to recover from surgery so using this analysis would not delay treatment.
Now, Claudio and partners at UMMC, Allegheny Health Network in Pennsylvania, Marshall University and hospitals in West Virginia are working to develop a clinical trial using ChemoID to help guide therapy recommendations. If approved, the trial could take about three years, Claudio said.
The groups hope to offer a double arm study that will follow patients who receive the current standard of care and those whose treatment is guided by results of the ChemoID assay of their tumor.
Claudio also is exploring use of ChemoID with ovarian, lung and breast cancer cells.


