Removing hurdles: With common goals, institutions agree to be ‘friends’
(Banner photo above: Sriramya Tata, left and Tara Rickman, biorepository specialists, prepare tissue samples for the UMMC Biobank.)
No academic medical center can afford to be an island, not when the worlds of research, education, and patient care change so fast.
When it comes to fulfilling the institution’s three essential goals, the University of Mississippi Medical Center is certainly not isolated as it contributes its expertise to other hospitals, clinics and schools, and benefits from theirs.
RESEARCH
By Karen Bascom
Open up a peer-reviewed journal or attend a scientific talk and you’ll likely find long lists of names, not just of investigators, but of their respective institutions.
Researchers create informal affiliations regularly, said Dr. Richard Summers, associate vice chancellor for research. These could be through “grassroots” networking opportunities or “meetings where they discover common interests and different skills,” he said.
For UMMC, formal affiliations and agreements between organizations don’t preclude these personal networks. Instead, they bolster these connections.
Institutional affiliations are “agreements to be friends,” Summers said. “One of the purposes is to lower the hurdles to developing contracts and sharing materials and resources.”
This is particularly the case for UMMC’s prominent relationship with the Mayo Clinic in Rochester, Minnesota. In 2010, the medical centers signed a long-term plan that includes conducting clinical research studies together.
The complexity and changing nature of science make institutional collaboration necessary. Trying to make groundbreaking discoveries alone is like playing baseball with a team made up of just pitchers.
“Nowadays, science requires more resources and technology, and one institution may not have all of the technologies, disciplines and expertise needed to conduct the work they want to do,” Summers said.
For example, Mayo and UMMC plan to study pharmacogenomics, or how the body processes medications, using patient data from the electronic health records system Epic. UMMC has used Epic since 2012, while Mayo is learning the ropes switching from their own in-house system.
“Large-scale affiliations also set the framework for ongoing person-to-person collaborations,” Summers said.
Dr. Tom Mosley, director of the MIND Center and an Alzheimer’s researcher, and Dr. Gwen Windham, professor of medicine and a geriatrician, will work with Mayo researchers on the Mississippi-Mayo Clinic Study of Aging. The team will implement advanced imaging techniques and population-level data to look for factors associated with mild cognitive impairment and dementia.
Other highlights of the Mayo affiliation include the UMMC 10K Project and a cooperative Clinical Trials Unit scheduled to open in the adult hospital in early 2019.

UMMC is reaching out to other medical centers as well. Earlier this year, a strategic affiliation with Vanderbilt University Medical Center opened the door for clinical research collaboration, among other missions. The institutions already work together through the NIH’s All of Us precision medicine initiative.
Affiliations with local hospitals also strengthen research. Methodist Rehabilitation Center has allied with UMMC through an affiliation agreement that will facilitate translational research in neuroscience. There’s also a relationship with the G.V. “Sonny” Montgomery VA Medical Center, which includes sharing of some faculty scientists and undergoing research regulatory components together.
As the state’s hub for biomedical research, UMMC works with colleges and universities, boosting access to mentors and technologies. The National Institutes of Health funds the Institutional Development Award program, which builds research capacity in states with historically low NIH funding. One of these programs, Mississippi INBRE, builds a network that connects faculty and students with UMMC’s molecular biology and genomics research facility.
Science is a team sport. Through these affiliations and others, UMMC has built a strong bench to support research in the lab and beyond.
-------------------------
EDUCATION
By Gary Pettus
Physicians who train at UMMC know they will see many patients with rare diseases and other conditions calling for highly specialized care.
But what about a case of, say, an inflamed gall bladder or shoulder pain or other complaints encountered more often?
To make a comparison: Even race car drivers have to get off the track eventually and drive their Civics to the store.

“We don’t want our trainees to become more skewed toward the unusual,” said Dr. Loretta Jackson-Williams, vice dean for medical education and professor of emergency medicine. “We want balance.”
To that end, UMMC’s various affiliation agreements help put trainees on the road more traveled. By working in hospitals and clinical settings beyond the Medical Center, these learners are able to explore the “breadth” of their specialties, Jackson-Williams said.
For the purposes of this article, affiliations will refer to the formal, institution-wide relationships involving the Medical Center.
Beyond these relationships, many schools at UMMC have forged their own outside agreements, said Dr. Ralph Didlake, associate vice chancellor for academic affairs. “There are just under 100 of these.”
When it comes to advancing the education mission here, the more formal affiliations benefit residents in particular.
One of whom is obstetrics-gynecology resident, Dr. Jaleen Sims, who has about one month left on her four-month rotation at Forrest General Hospital in Hattiesburg.
“The exposure here is outstanding. We may have up to 15 to 20 surgeries in a week.” For Sims, each “week” in Hattiesburg is four days; she then returns to Jackson for clinic on Fridays.
“We’ve done several vaginal hysterectomies, which are typically scarce at the university,” said the Kansas native now living in Flowood. “I wouldn’t feel very confident doing them once I’m out in practice if I had not come to this institution. I’ve also been able to do abdominal and laparoscopic hysterectomies, as well as pelvic floor reconstructions.
“If I end up at an institution without a urogynecologist, I’ll be able to perform those surgeries as well. The repetition here really prepares for the day we go into our own practices.”

OB-GYN residents spend four months at North Mississippi Medical Center in Tupelo as well, said Dr. Elizabeth Lutz, assistant professor of obstetrics and gynecology and associate residency program director in the School of Medicine. At St. Dominic Memorial Hospital in Jackson, they do one month during their second year and one more during their third.
Although residents visiting St. Dominic assist primarily with very sick cancer patients, in Tupelo and Hattiesburg they experience a greater number of “normal” cases, Lutz said. “We don’t do a ton of normal cases here.”
With longer rotations in Tupelo and Hattiesburg, residents have the opportunity to do more procedures, she said. “They operate a lot; it’s great for them, and they love it.”
That’s all true for surgeons-in-training as well, said Dr. Mark Earl, associate professor of transplant surgery. Each month, two different residents take on cases at NMMC, and two more at Baptist Medical Center in Jackson. This goes on for 12 months of the year.

“Both of those hospitals provide high-quality surgical care,” Earl said. “The surgeons there do high-volume work and have an interest in education.
“It’s a great way for our residents to have an experience at a private-practice institution. They get excellent, excellent training.
“At the Medical Center, we see a lot of very complex surgery, very sick patients and a large amount of trauma. These other places see a lot of complexity, too, but they also have a large volume of elective general surgery.
“This gives our residents depth, adds to the number of cases available to them, and adds to the number of different people who train them.”
All of the hospitals helping train UMMC’s residents have at least two things in common, Lutz said: “High volume and great reputations in the state.
“The surgeons there are very interested in education; they are motivated. This is a service they do to educate our residents. And we’re very thankful.”
------------------------------
PATIENT CARE
By Ruth Cummins
Patients on the Mississippi Gulf Coast and in Tupelo don’t have to leave home to receive treatment from UMMC caregivers, thanks to several formal affiliations.
Soon, some patients from Meridian won’t have to travel to Jackson either.
“The future of health care in Mississippi is one that is founded on collaboration and cooperation among the in-state systems,” said Kevin Cook, chief executive officer of the UMMC Health System.
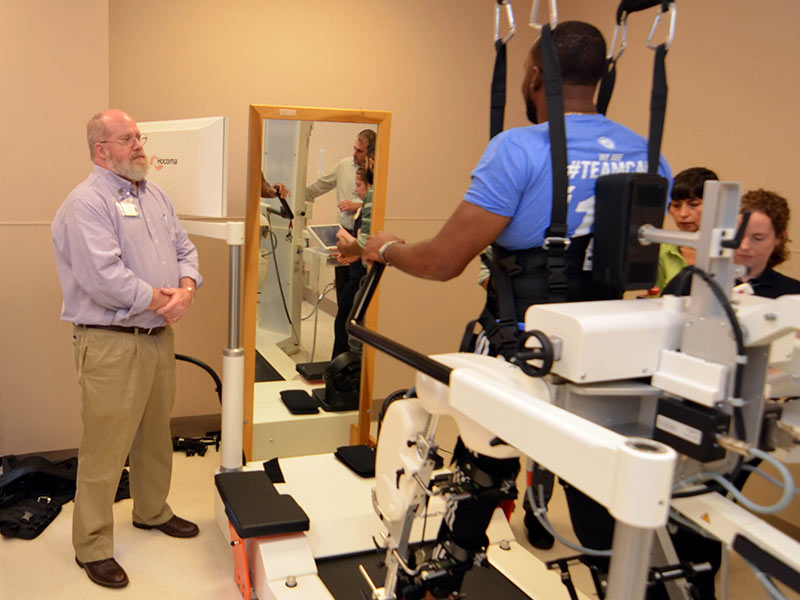
In the Medical Center’s own backyard, a 2014 affiliation with Methodist Rehabilitation Center has allowed the systems to build on each other’s strengths. Patients are receiving enhanced care for stroke, brain and spinal injuries, movement disorders and other neurological conditions.
UMMC has expertise in clinical orthopaedic and neuro-trauma care, neurology and neurosurgery. MRC is a nationally recognized, private nonprofit rehabilitation hospital that treats disabling injuries and illness.
The agreement integrated UMMC’s patient rehabilitation programs into MRC, a seven-story rehabilitation hospital on the Medical Center campus.
In Tupelo, about a three-hour drive from Jackson, the 2015 partnership between UMMC and North Mississippi Medical Center focuses on a pediatric clinic offering cardiology and endocrinology care through Children’s of Mississippi, a part of UMMC that encompasses all of its pediatric services as well as Batson Children’s Hospital.
The partnership features a pediatric hospitalist with Children’s of Mississippi who provides care for children at NMMC’s pediatrics unit.
“We are the state’s children’s hospital, and that carries responsibility to the whole state. It’s not just about Jackson,” said Guy Giesecke, CEO of Children’s of Mississippi.
In east-central Mississippi, UMMC and Anderson Regional Health System in Meridian embarked on an affiliation in December 2017; it will provide local access to UMMC physician subspecialists, especially pediatric subspecialists.
Anderson Regional has the only inpatient pediatric services in the Meridian area and provides pediatric physical, occupational and speech therapy. The Meridian system includes a 400-bed hospital that houses centers of excellence in cardiac services, oncology, surgical services, women’s health, rehabilitation and more.
On the Mississippi Gulf Coast, UMMC teamed up in January with Gulfport’s Memorial Hospital to care for the region’s smallest and sickest newborns. Children’s of Mississippi manages Memorial’s 23-bed neonatal intensive care unit, the Mississippi Gulf Coast’s only Level III NICU. UMMC’s main campus in Jackson is home to the state’s only Level IV NICU, the highest level.
UMMC also provides a pediatric hospitalist for Memorial.

Beyond Mississippi, UMMC and Vanderbilt University Medical Center in February announced a strategic affiliation that allows the two institutions to form and share new clinical programs and services, enabling them to formally work together on a broad range of health and wellness programs.
“As the leading academic medical centers in our respective adjoining states, we also face many of the same or similar opportunities and challenges in today’s changing health care landscape,” said Dr. Charles O’Mara, UMMC associate vice chancellor for clinical affairs.
UMMC is nationally recognized for its advanced telemedicine program and for its clinical services, while VUMC is similarly recognized for its advanced clinical care.


