Novel procedure restores ability to eat, quality of life

When you chew and swallow a hamburger or apple, you expect the food to travel to your stomach without pain or much ado.
But when the esophagus doesn’t properly squeeze food down – and the lower esophageal sphincter muscle doesn’t open properly so that food can continue its journey to the stomach – the food gets stuck and you have a problem. It backs up into your mouth, causing chest pain, vomiting and weight loss, and if it happens when you sleep, there is danger of aspiration into the lungs.
Surgeons at the University of Mississippi Medical Center are offering long-term relief for patients suffering from achalasia, an often chronic disease that can rob patients of quality of life and result in malnutrition and dehydration. “We can give that food clear passage,” said Dr. Jacob Moremen, assistant professor of surgery and a member of the Interdisciplinary Thoracic Team at the UMMC Cancer Institute.
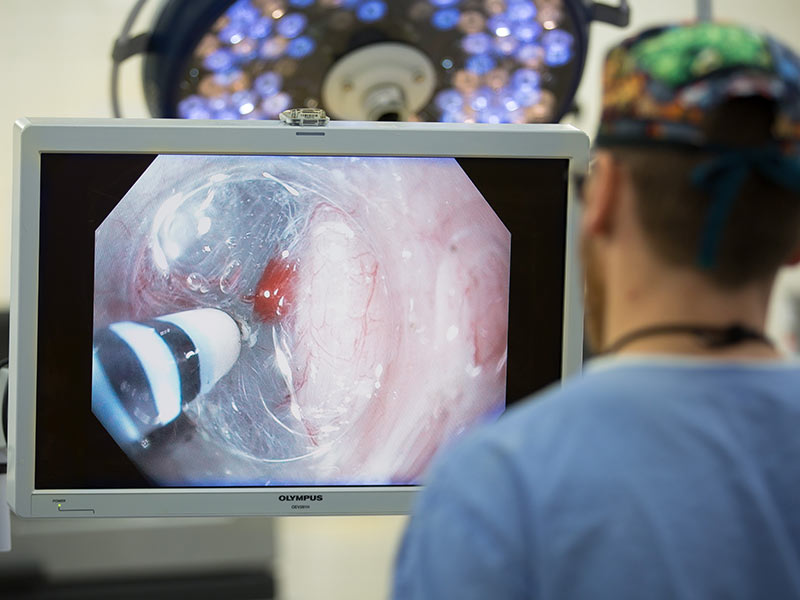
He performs a new minimally invasive procedure called peroral endoscopic myotomy, or POEM, an incisionless alternative to the current surgical standard of laparoscopy. “It’s done through a scope that goes in the patient’s mouth and down the esophagus without cutting the skin,” Moremen said. “The procedure divides the muscles at the end of the esophagus to open the obstruction.”
UMMC is the only provider offering POEM in the state, said Dr. Christopher Anderson, professor and James D. Hardy Chair of the Department of Surgery. Moremen has performed 10 of the procedures since December 2016, and five patients are awaiting their surgery.
POEM “works about as well or similarly to surgical myotomy. It gives the patient the chance not to have surgery,” said Moremen, one of a handful of physicians in Mississippi who perform the procedure. “It takes them from not being able to swallow food at all and having pain in the chest, to being able to eat as close to normal as they ever did.”
POEM surgery in August 2017 took Pontotoc resident Audra Odom from a miserable existence to a life that allows her to do something that most people take for granted: eat normally.

“Sometime at the beginning of the summer, all of a sudden I couldn’t keep anything down. I couldn’t keep saliva down,” said Odom, 46.
Odom finished law school in December 2016 and was set to take the bar examination in July 2017. Instead, she found herself in the hospital, badly dehydrated and malnourished. “I went back and forth to doctors for the first couple of months” before her diagnosis of achalasia, she said.
She lost 70 pounds in three months, but was overweight before her symptoms became severe, Odom said. Her family medicine doctors in Tupelo referred her to UMMC.
She remembers telling Moremen that the thing she missed most was being able to keep down ice water. “I’d drink a Slushie and throw up ice. That’s how quickly it came back up,” Odom said.
Achalasia is a fairly rare disease, Moremen said. The prevalence is about one or two new cases per 100,000 population, about half as many new cases each year as esophageal cancer, which itself is uncommon. “We don’t know what causes it. I can’t blame it on behavioral factors like poor diet or cigarette smoke,” he said. “It’s fairly random, and there’s not a typical patient who gets it.”
The decision on when to treat achalasia is different for everyone depending on their tolerance of the symptoms. As the disease progresses, some patients will “self-select” their diet and eat only things that best stay down. “They might stop eating bread, then stop eating ground beef,” Moremen said. “They might just eat soup. This tends to go on for some time before going to their doctor. Then it may take weeks to arrive at the correct tests needed to diagnose it. It’s not always quick.”
The procedure itself has a steep learning curve, something that Moremen studied for some time before performing his first POEM. And although the procedure is considered difficult, recovery is not.
“We keep patients overnight because it’s a relatively new procedure,” he said. “For the most part, everyone goes home the next day, and can at least consume liquids right away. Short of a little chest discomfort from the dividing of the muscles, it’s like having a typical upper endoscopy.”
Patients generally are diagnosed by their gastroenterologist, who refers them to the Medical Center.
“The procedure is very little known outside of academic circles and some of the most cutting-edge private groups,” Moremen said. “Everyone who’s been through medical school has heard of the disease, but many physicians just don’t have their radar up for it because of its rarity. Often patients are frustrated because they can’t swallow and keep losing weight until someone figures it out.”
Patients are usually delighted to find they can feel the results immediately. “People come in almost unable to swallow. But after the procedure, they say they can tell a difference right away,” Moremen said. “Eating is so fundamental to the human experience.”
After Moremen performed the POEM procedure, Odom said, she was afraid to eat. “I’d been throwing up for four months,” she said.
Moremen “said I could drink some water. I did, and it stayed down. It was weird. I sipped water for the next day,” Odom said. That was followed by clear broth for a week, then thicker soups and pudding. “It took about a month before I could have just about anything,” she said.
There are some tradeoffs, but Odom gladly accepts them. “I can’t eat a lot at a time, and I have to eat slowly,” she said. “I can’t lie down for two hours after eating. I can’t have a late-night snack. And I still get nervous about eating.
“Finding out about it and having the procedure has been a blessing,” Odom said. “I can’t say enough wonderful things about Dr. Moremen and my family medicine residency center in Tupelo. Life is better immeasurably – for everyone.”


