For some, transplant best liver cancer therapy

Published in News Stories on September 29, 2016
Jessie Wallace points to the University of Mississippi Medical Center transplant team as the one that made it possible to beat cancer and do so closer to home.
The Brandon resident, 75 when she had a liver transplant in June 2015, is the oldest patient to receive a new liver since UMMC restarted its transplant program in 2013, said her transplant surgeon, Dr. Mark Earl.
Hepatitis C likely led to Wallace's cancer, said Earl, associate professor of surgery. “Most people who have transplants have liver disease through no fault of their own,” he said. “They may develop hepatitis through blood transfusions.”
Wallace had cirrhosis, a slowly progressing disease, in which scar tissue replaces healthy liver tissue. Hepatitis C, fatty liver and alcohol abuse can cause it.
“Right now, we're at the peak of folks who got hep C from blood transfusions in the early 80s before the virus was identified,” Earl said. Since the virus was identified, blood has been screened for hepatitis C before it's offered for transfusion.
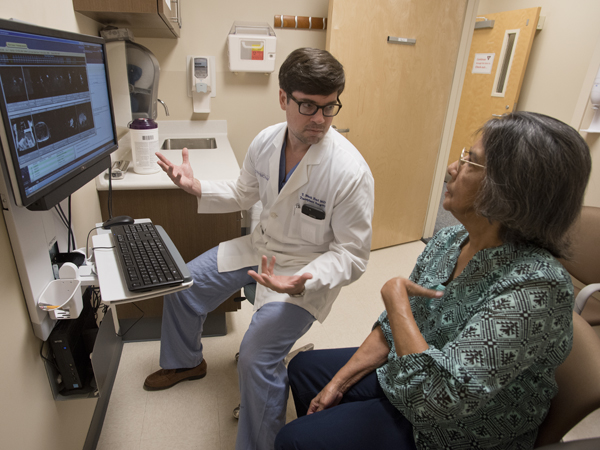
Dr. Mark Earl shows Wallace images of the cancerous liver he and his team removed and the new one that she received.
But Wallace wasn't so lucky. A spate of health problems years ago led to a blood transfusion, the likely cause of her hepatitis C. Down the road, it led to cirrhosis and then liver cancer.
She's in a small group of people for whom a liver transplant can be offered as a cancer cure, Earl said. “This is only for early stage disease.”
If liver cancer has spread to other organs, a transplant is fruitless.
But Wallace was a good candidate. “She was 75 but her physiological age was much younger,” he said.
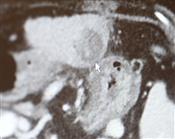
A recent visit with Earl started and ended with a hug. As they examined MRI's of her then-cancerous liver and those of her new one, Earl commented, “You are the living proof that chronological age means very little. Biological age matters more. Biologically, you're like a 55-year-old.”
“I'm still going,” Wallace replied.
“I know. I know. You're amazing,” Earl responded.
Wallace now sees transplant hepatologist Dr. Brian Borg for her follow up care.
Wallace said she doesn't remember having symptoms of liver cancer but admits her family saw some yellowing of her eyes, a sign her liver wasn't functioning properly, and she had lost weight. Her cancer was caught on a routine visit.
“After my doctors at GI Associates saw a spot on my liver, they sent me to Dr. Earl,” she said. “After some X-rays he said it was cancer. They gave me chemo but it didn't work and then he said it would be a good idea if I'd have a liver transplant.
“I was scared to death when Dr. Earl was talking to us. I was shaking,” she said.
Tests on her organs and function kept giving the greenlight, so she soon joined the liver transplant waiting list.
“In April I had the tests and in June I had my surgery,” she said.
Today, she takes anti-rejection medications but with a new liver, no longer has hepatitis C, cirrhosis or cancer. She's returned to her part time job as a cashier at Dollar General in Brandon and laughs when she says she has no hobbies.
“I don't have time to do anything,” she said, pointing to 13 grandchildren and eight great-grandchildren who “keep me busy, keep me running.”
She's one of the lucky ones, said Earl. Her cancer was caught early enough.
The transplant team, of which he is a member, expects to complete about 40 liver transplants in 2016 and will complete its 100th liver transplant since the program's rebirth before the year ends.
Earl cites parallels between the fundamentals of building a transplant program and treating cancer - both rely on multiple specialists working together to achieve what's best for the patient - as strengths of the transplant/cancer therapy.
Having a transplant to treat liver cancer is an option for very few people who annually are diagnosed with the disease, he said. “Most have a disease so advanced, they would not tolerate the surgery.”
If imaging shows they are candidates, the team begins the search for a new liver and starts cancer therapy at the same time. Most liver cancer is diagnosed with imaging.
UMMC Cancer Institute doctors use imaging to diagnose liver cancer and to follow therapy progress.
The need for transplants is likely to grow. Hepatitis C-fueled liver cancer will decrease in the next decade due to improved treatment, said Dr. Christopher Anderson, professor and chair of the department of surgery and its division of transplant surgery.
But the need for transplants for liver cancer may increase. While the occurrence of hepatitis C will decrease, a new risk factor is overtaking it: Fatty liver disease.
In a state whose population wins the unwanted title of perpetually being the most overweight in the nation, fatty liver disease can lead to more cirrhosis and that is a primary risk factor for end-stage liver disease and for hepatocellular carcinoma, a dominant type of liver cancer.
Fatty liver disease will be the leading indication for liver transplant within the next 20 years, Anderson said.
Anderson
Currently, from 15 to 20 percent of liver transplants in the Southeast and at UMMC are for liver cancer, Anderson said, adding he expects that to rise to a consistent 20 percent or a little higher.
The UMMC Cancer Institute's hepatobiliary team, a big name for a group of specialists, also cares for many liver cancer patients who are not transplant candidates.
“Part of a liver transplant program is having a liver tumor program,” Anderson said. “Each patient is seen by someone fellowship trained in hepatobiliary surgery. The disease is discussed at a multidisciplinary conference. The whole team is here to figure out how we care for the disease these people have.”
Teams include the surgeons Anderson mentioned, hepatologists, medical and radiation oncology physicians, radiologists, pathologists, nurses, clinical trial coordinators, therapists and others as needed.
“For patients who don't qualify for a transplant, we offer the whole gamut of other treatments,” he said. “We offer a personalized treatment plan that is pretty aggressive for each patient.”

Earl gives Wallace a hug as a recent visit ends.
Having the transplant program here means Mississippi patients do not have to be referred out of state for the live-saving therapy and lifetime of follow up appointments.
The goal isn't one his team can accomplish without help from organ donors.
“There are not enough donors for the demands of liver transplant,” Anderson said. The Mississippi Organ Recovery Agency does a good job, he added. “We just need more donors.”
With more donors, more people like Wallace can look forward to a cancer-free survival.
Photos
 | Donate to the Professional Development/Student Travel Fund Use the form below to make a donation to the School of Graduate Studies' Professional Development/Student Travel Fund. Your support is greatly appreciated. High Resolution Medium Resolution Low Resolution |
 |
High Resolution Medium Resolution Low Resolution |
 | Donate to the Dean's Fund Use the form below to make a donation to the Dean's Fund in the School of Graduate Studies. Your support is greatly appreciated. High Resolution Medium Resolution Low Resolution |
 | 2016 Reunion 1.jpg High Resolution Medium Resolution Low Resolution |
 | Class of 1966.jpg High Resolution Medium Resolution Low Resolution |


