Second chance at life: Surgeons rebuild cancer patient’s jaw
When Almarie Maldonado Pagan noticed a lesion inside her mouth on her left jawbone in October 2020, the busy high school senior and her mom weren’t too worried.
“We didn’t think it was cancer,” said Maria Pagan, mom to 17-year-old Almarie. “We just thought we could get it removed and continue on with life.”
But when the lesion became a large growth in just a few weeks’ time, Almarie’s endodontist suspected cancer. He advised her parents in mid-November, even before getting the results of a biopsy, to take her to specialists at the University of Puerto Rico Medical Sciences Campus in San Juan. Overnight, life changed for the family of four living in Manati, a city on Puerto Rico’s northern coast.
Almarie was diagnosed with an aggressive and uncommon bone cancer, one that put her life in immediate danger. Delaying treatment for her osteosarcoma wasn’t an option.
As Almarie lost weight and the ability to eat and her pain intensified, one of her providers in early December reached out to Dr. Ignacio Velasco-Martinez, assistant professor of oral and maxillofacial surgery at the School of Dentistry at the University of Mississippi Medical Center.
Almarie’s pediatric oncology caregivers “looked for a provider for her on the island, but nobody wanted to do the surgery,” said Velasco-Martinez, a native of Chile who performed his surgical residency at the University of Puerto Rico Medical Sciences Campus.
“It was so complicated in every aspect: removing the cancer, and reconstructing her jaw in a very sensitive region. It was going to be a radical surgery.”
“The tumor was growing very fast. It was bigger every time we saw her,” said Dr. Irelsy Rivera, a fourth-year oral and maxillofacial surgery resident at the University of Puerto Rico Medical Sciences Campus who performed rotations with Velasco-Martinez when she was a dental student.
Almarie was admitted to the hospital for pain and nutrition support, but “we needed the tumor managed as soon as possible, and I remembered Velasco,” Rivera said. “He was someone I could reach without hesitation, and I knew he could treat her well.”
Velasco-Martinez quickly set into motion a plan to bring Almarie to UMMC in Jackson for complex surgery that would require the skills of multiple experienced specialists. The first step, though, was chemotherapy as a prelude to a surgery that would involve removing 80 percent of her mandible, or jawbone, and reconstructing it with bone from her own fibula.
The devastating diagnosis couldn’t have come at a worse time for Almarie, a volleyball player and Netflix fan, and her family. “Two days before we found out Almarie had cancer, my mom’s dad died. She was still numb,” said Linda Maldonado Pagan, Almarie’s 24-year-old sister.

“I was in disbelief. I was shocked,” Almarie’s mother said. “I had to process it.”
Almarie’s chemo began Dec. 11. Velasco-Martinez consulted with Almarie and her home medical team via telehealth on Dec. 29. Her UMMC surgeons would be Velasco-Martinez for removal of the cancer, and plastic surgeons Dr. Benjamin McIntyre and Dr. Laura Humphries for reconstructing Almarie’s jaw, chin and neck.
The timetable was pushed up, though, after a CT scan showed that the chemotherapy wasn’t working. “It was growing and becoming more painful,” Velasco-Martinez said. “It would get to the level where it couldn’t be treated by surgery. It would be fatal.”
On Jan. 25, her surgeons set Feb. 10 as the date for her operation. Almarie and her family made the 1,750-mile trip to Jackson, meeting with the surgery team face-to-face for the first time on Jan. 28.
“The first time I saw her, the tumor was the size of a tennis ball. The second time I saw her, three or four weeks later, it was the size of a softball,” said McIntyre, associate professor of plastic surgery whose practice includes reconstructive microsurgery of the head and neck. “She couldn’t open her mouth. She was in considerable pain.”
She’d already lost her beautiful dark hair to the chemo. Almarie understood the toll surgery would have on her face, and that there would be more surgeries and chemo in her future.
“At first, I was scared,” she said. “I was afraid I wouldn’t be able to walk again. But when they explained how it would work, I knew it would be for the best.”
“She was scared, and she was very brave,” McIntyre said. “She knew that this would kill her if she didn’t have the surgery.
“She wanted to try and live.”
Highly malignant tumors of the bone are uncommon. Almarie’s particular tumor was exceedingly rare. “Osteosarcomas of the mandible represent 7 percent of all osteosarcomas and 1 percent of all head and neck malignancies,” Velasco-Martinez said.
For Almarie’s special and complex circumstances, Velasco-Martinez, McIntyre and Humphries worked with a vendor to create a simulated virtual surgical plan. Surgeons often take advantage of virtual surgical plans because they can so precisely recreate the patient’s anatomical structure, and because they allow the surgery team to visualize the reconstructive work ahead.

Using Almarie’s imaging, the surgery team worked with biomedical engineers to produce pre-operative and post-operative models of Almarie’s skull and jaw, the first marked by her tumor, the second showing the placement of her fibula bone as part of the jaw’s reconstruction.
A separate set of models guided them through the location of nerves, where to make cuts in removing most of her jawbone, and fashioning a new one from her fibula.
“I tried to do the surgery a thousand times in my head,” Velasco-Martinez said. “We used the models to explain the surgery to the patient and her family.”
The models also took in another unusual aspect of the surgery, Humphries said: It would require not one, but two flaps as part of the reconstruction. Flap surgery involves transporting live, healthy tissue from one location of the body to another that’s in need of skin, fat, muscle or bone.

The removal of part of Almarie’s fibula to create a new jawbone was the first flap. The second flap was using skin from her thigh to recreate her chin and part of her neck.
Almarie’s family stayed in a hotel as the days ticked down to the Feb. 10 procedure. Social workers and members of the medical team “made sure we had everything we needed,” Linda said.
“They knew we came from so far away. They were so attentive, especially when we were in the hospital. We could only have two people in the room with Almarie, but they made adjustments so that her dad (Alfredo Maldonado) could see her, too.”
The surgery lasted 11 hours.
“While Dr. Velasco-Martinez was working on excising the tumor, we dissected the fibula bone,” said Humphries, assistant professor of plastic surgery whose practice includes children’s craniofacial, trauma, plastic and reconstructive surgery.
“Everything flowed so that we could work efficiently together. Because we had a surgical plan, we knew where we wanted to cut the bone, and we were able to move the bone with its blood supply and vessels to Almarie’s face.”
McIntyre and Humphries reattached vessels and nerves using microsurgery, a tool used by many plastic surgeons when transferring tissues from one part of the body to another or when reattaching severed parts of the body. They used specialized instruments under a microscope as they constructed a new jaw for Almarie, preparing the site for future surgeries, such as giving her dental implants.
“I was able to harvest a flap of skin from her leg to cover the outer surface of her chin and neck,” Humphries said. “The first flap also had a skin component to cover her mouth and tongue.”
Almarie’s mom said she was anxious when her child was wheeled in to surgery, “but I felt a calm because of Dr. Velasco-Martinez’ reassurances. And, the nurses called us every hour with an update.”
“There will be more surgery in the future, but it was a complete success,” Velasco-Martinez said. “There have been no complications. We were able to remove the entire cancer.”
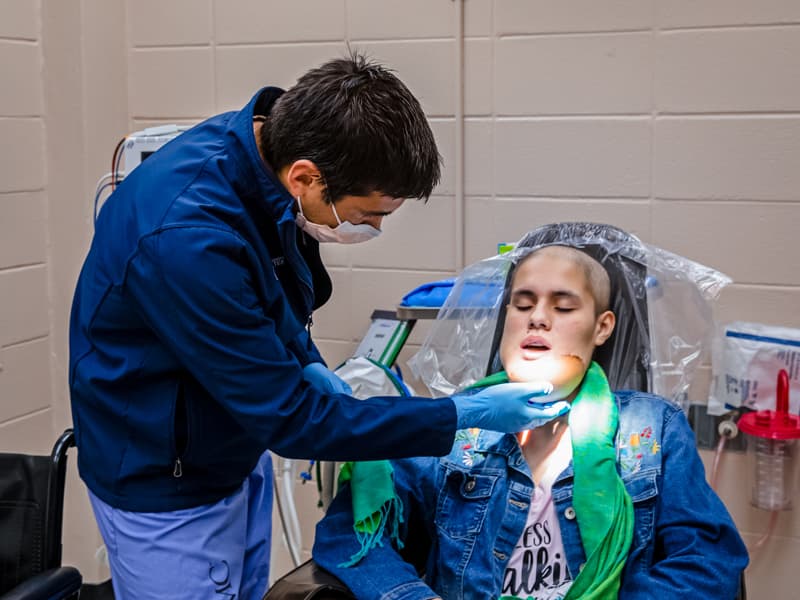
After a five-day stay in the new Children’s of Mississippi Pediatric Intensive Care Unit, Almarie was discharged following a few days in a regular room. On March 9, she saw her surgeons during a follow-up appointment in the School of Dentistry oral and maxillofacial surgery clinic.
“When are you guys going back home?” McIntyre asked Almarie, her mom and sister.
“She wants to take you with us,” Linda told him as Almarie grinned.
Almarie will have chemotherapy through her providers in Puerto Rico before returning to UMMC in six months for another surgery to give better contour to her chin and lower face. She also will have speech therapy at home and help with transitioning from liquids to solid foods.
Ask Almarie how she’s doing, and she will tell you: “I’m fine.”
Her plans to study occupational therapy after graduation from Piaget Bilingual Academy in Manati are unchanged. “I’ve always been interested in OT, and this has reassured me,” she said of her surgery and recovery.
She will also get back to her hobby of cooking, especially “baking sweet treats,” her sister said.
When her surgeons floated the idea of Almarie having some of her future surgeries at home, Maria said, Almarie was having none of it.
“She said, ‘No! I want you to do it!” her mom said.
Before her appointment ended, Almarie’s surgery team surrounded her for a photo. “Can I take a selfie with you? I’m going to miss you!” McIntyre said as Almarie quickly leaned in for the picture.
It’s no wonder that Almarie was conflicted when it came to going home and having to leave behind, at least for now, the surgeons whose skilled hands and big hearts saved her life.
“I love them! I love them!” she said.


