UMMC change managers inspire consistent delivery, excellent care
You don’t have to be a manager at the University of Mississippi Medical Center to be passionate about change management.
What you do need, though, is a commitment to provide consistently excellent and safe patient care, and the desire to drive significant, lasting change throughout the 864-bed UMMC Health System, be it in enhanced operations or stable finances or zero patient harm.
“Change management offers a way for everyone to think smarter about the way we work, but it must start with senior leadership,” said Chief Medical Officer Dr. Michael Henderson. “Change management is the key lynchpin for helping drive improvement.
“It’s how you prioritize work and plan and set up projects, implement them and inspire people to be engaged in them, and then sustain them for the long term,” he said.
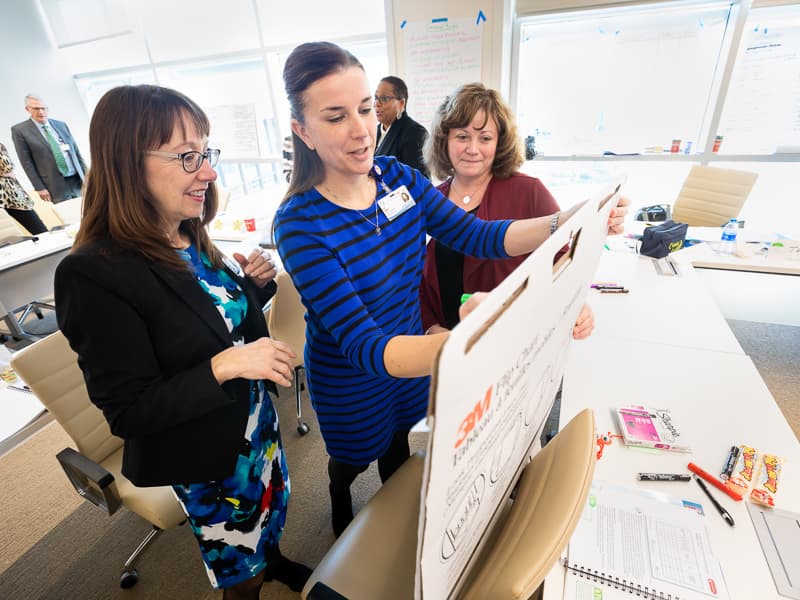
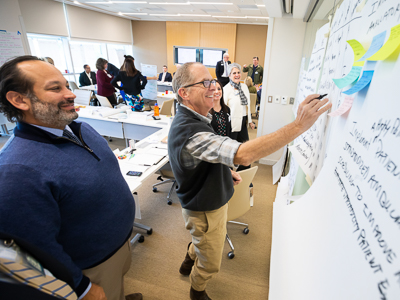
Leaders set the tone, and the Medical Center last week offered two-day training to give 50 of them tools for facilitating change needed to make UMMC its best self. Those trained represent a multitude of areas, clinical and non-clinical, including telehealth, human resources, the Division of Information Services, quality performance, physicians, department chairs, finance, business operations, UMMC Grenada and UMMC Holmes County.

A small example of one tool that leaders across campus can use to make operations more smooth and efficient when there are only so many hours in the day: Be smart when facilitating meetings.
“We need a more standard way of setting up more useful and productive meetings so that we don’t waste a lot of time,” Henderson said. “The key to that is pre-planning, having the right people there, and having appropriate follow-up. What needs to be done? Who needs to do it, and by when?”
Another tool is the ability to best communicate with coworkers. “Everyone wants to be communicated to, but not necessarily in the same way,” Henderson said. “Some want it face to face. Some want it in emails.”
The long-term goal, he said, is “to get everyone more engaged in performance improvement and to understand that this is the UMMC way of doing business.”

The Medical Center receives guidance through the Joint Commission Center for Transforming Healthcare. The center helps leaders to transform their organization to one of high reliability, which means consistent excellence in quality and safety across all services maintained over long periods of time.
The reasons for driving change are much broader than improving performance on quality measures such as hospital-acquired infections, medical errors, hand hygiene, patient experience and overall patient safety. UMMC has made great strides since Henderson joined UMMC as CMO in 2015.
Hand hygiene compliance jumped from 54 percent in 2015 to 83 percent today. Hospital acquired infections fell from an average 54 per month to 20. And, patient safety indicators – adverse and largely preventable complications that patients can experience in a health care setting – fell from 32 per month down to 9.
“Quality improvement helps us on so many fronts, including operations, finance, workforce engagement, institutional reputation, and most importantly, patient experience and outcomes,” said Dr. Charles O’Mara, associate vice chancellor for clinical affairs. “We’ve made significant progress in transforming our culture to one that is a safe environment for patients.”
That’s thanks in part, O’Mara said, to significant progress in leadership engagement, from interaction with the governing board, the Institutions of Higher Learning, “all the way to the front-line providers doing the hard work of health care on a day-to-day basis.”
Change management, Henderson said, is “another step” in the Medical Center’s journey to high reliability, one that broadens beyond a culture of safety and a focus on patient experience. “Our leadership wants to do that here,” he said. “This is potentially the step we take so that we can focus on what we will fix this year in operational spaces and financial spaces.”
It means uniformly applying the methods for performance improvement across the health system, O’Mara said, to impact both clinical and non-clinical areas like finance, legal, contracts, education and research.
“This phase is to engage the leaders, and the leaders convey this methodology to the people they work with,” O’Mara said. “It filters out from there.”


