Rural opioid disorder patients benefit from in-person, telehealth visit combo

It’s hard enough for opioid addicts to seek help and stay the course, but it’s especially tough for people in rural areas who don’t have local addiction treatment services, much less a physician to guide their care.
But using a combination of telehealth and in-person clinic visits, the addiction team from the University of Mississippi Medical Center’s Department of Psychiatry and Human Behavior in collaboration with the UMMC Neuro Institute is tailoring treatment to reach and support patients where they are. It’s an initiative that not only can save lives, but that in time could emerge as a national treatment model for people coping with opioid addiction.
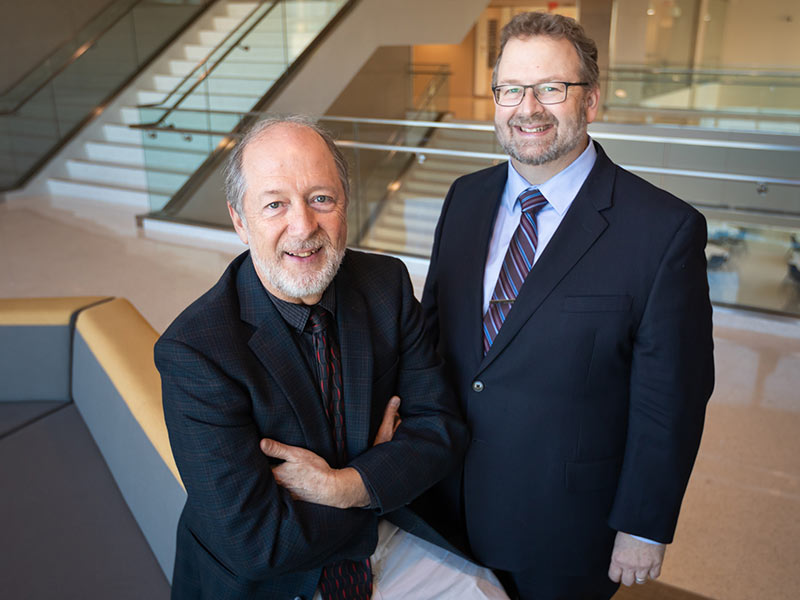
“We will identify patients with opioid disorders who don’t have these interventions,” said Dr. Jefferson Parker, professor of psychiatry, who with psychiatry professor Dr. James Rowlett is using a $1.8 million yearly grant to create the treatment program. “There are patients who need this and who are sitting in jail because there is no treatment available.”
The approach is called TeleMAT and will use medication-assisted treatment, or MAT, to help free patients from addiction. The medications include drugs that reduce cravings for opioids and prevent addicts from getting high if they relapse.
The two-year grant comes from the state Department of Mental Health, with parent funding from the U.S. Substance Abuse and Mental Health Services Administration. UMMC and the Department of Mental Health will work together to identify patients who lack services for treatment of opioid disorders.
UMMC will provide care from psychiatrists, psychologists, social workers, nurse practitioners and others on the addiction team. Patients will make clinic visits to Psychiatry’s Behavioral Health Specialty Clinic at the Jackson Medical Mall, followed by visits with an addiction team member through a live connection facilitated by UMMC’s Center for Telehealth.
The Department of Mental Health will use additional grant money from the federal agency to help patients visiting the Jackson clinic with lodging and transportation. And, UMMC will use a portion of its grant funding to implement an education curriculum for patients, and to help those who can’t afford their medications.
The two-pronged approach targets patients with moderate to serious addiction, Rowlett said, in addition to those who may use opioids sporadically, yet lead a mostly stable life. They will be referred through routes including family physicians, DMH regional clinics, or even state-sponsored drug courts for offenders who are given the chance to undergo drug treatment and counseling in hopes of avoiding jail time and rebuilding their lives.
Treatment teams from UMMC and DMH will decide the best course of action for each patient, Rowlett said. “We will develop a treatment plan and propose it to the patient,” Parker said.
Depending on the patient, the addiction team may prescribe naltrexone or buprenorphine/naloxone. Naltrexone works in the brain to prevent feelings of well-being, or a high, for opioid users, and it decreases the desire to take opiates. Buprenorphine, packaged with or without naloxone, works to prevent cravings and withdrawal symptoms in someone who stops taking opioid drugs.
Addiction psychiatrists and other prescribers not only must possess a special license and waiver to prescribe the medications, but they also must have specific training. The Department of Psychiatry will use grant funding to hire an additional nurse practitioner and psychiatrist who are authorized to use MAT. The waiver allows a license-holder to prescribe to 30 patients per year, with the option of requesting an increase to 100 patients the second year, Parker said.
Patients will be followed via telehealth for monitoring of their prescription drugs and delivery of education and other addiction treatment. “Evidence shows that the results are better if you get both (in-person and telehealth treatment),” Parker said. “We don’t want to put someone on medications and then let them go about their business.”
To ensure privacy and confidentiality, telehealth visits generally will take place not in patients’ homes, but at regional mental health clinics. The first patients will be seen in early spring.
The need for TeleMAT is great, Rowlett said. “There were about 300 overdose deaths in the state in 2017, and in the first quarter of 2018, deaths were higher than in the first quarter of 2017. The good news is that prescriptions for opioids given for pain in Mississippi are down by about 20 percent.
“But despite the drop in prescriptions, the overdose death rate hasn’t slowed,” he said. “Users who can’t get a prescription just switch to street drugs like fentanyl and heroin.”
Dr. Saurabh Bhardwaj, assistant professor of psychiatry, has been offering MAT at the Specialty Clinic since last fall. He is UMMC’s first provider to offer the treatment, considered the national gold standard of care for opioid disorders. “We have several patients who are mothers with children who are successful with MAT,” Parker said. “One of them has been able to keep her newborn because of it. She’s now in a sober living situation.”
Since the Specialty Clinic’s creation, the addiction team has worked within and outside the Medical Center to identify and inform those who could benefit from treatment. “We’ve talked to our Emergency Department physicians about identifying patients,” Parker said. “They can come to our clinic promptly, if not the next day.”
While most treatment programs nationally target an urban population, “this is new,” Rowlett said of TeleMAT.”This is different. In Mississippi, most of the deaths are in the north, the south and Jackson, but we have lots of pockets with very few clinics.”
Parker and Rowlett will track participants and document their outcomes “based on rigorous science,” Rowlett said.
“We have a unique challenge,” he said. “The hope is that TeleMAT can provide a model for places in the nation with similar problems. This has hit a lot of rural places pretty hard.”


