RECOVER explores Long COVID

Some people catch COVID-19 and recover from the cough and fever quickly. Others spend months with persistent fatigue and trouble breathing.
They’re in it for the long-haul.
Now, a massive nationwide effort seeks to understand why. The University of Mississippi Medical Center is part of RECOVER (Researching COVID to Enhance Recovery), a study on who is most likely to develop Long COVID, and how to treat and prevent it.
The National Institutes of Health has dedicated nearly $470 million across the United States to conduct RECOVER. Led by New York University, the study will have hundreds of enrollment sites that expect to recruit more than 10,000 individuals for the study. UMMC received more than $566,000 from the NIH in late 2021 to begin its study site.
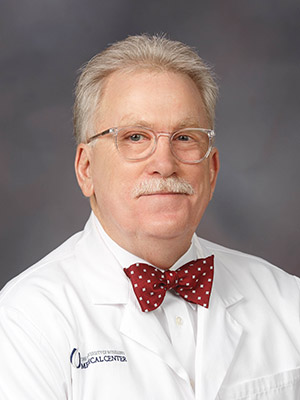
Dr. Gailen Marshall, R. Faser Triplett Chair of Allergy and Immunology, is the lead investigator for UMMC’s study site.
He says that earlier in the pandemic, the health and medical community “put a lot of focus on the acute phase of the disease.”
That included the development of effective treatments and vaccines. However, “It began to emerge that that some people who had been ill with COVID-19 to variable degrees had persistent symptoms,” he said.
These symptoms can include cough, breathing difficulty, aches, weakness, fatigue or cognitive dysfunction known as “brain fog.” When these occur 30 days or more after a COVID-19 diagnosis, it’s known as Long COVID.
“While most people with COVID-19 become well in 14 days, there’s an alarming number who are either still ill after more than 30 days, or they recover and then symptoms emerge or reoccur,” he said. “And it’s not just people who went to the intensive care unit. There are people who didn’t even go to the hospital who experience PASC.”
That’s short for post-acute sequelae of SARS-CoV-2, a term the medical community uses for Long COVID.
“The definition for PASC is intentionally broad,” Marshall said. “There are people who have a cough for one month, while others have a brain fog for three months.”
RECOVER aims to clarify some of the unknowns with Long COVID. Why do some people have much more serious cases than others? How does PASC differ among the virus variants? How do vaccinated individuals fare?
What we do know is that Long COVID a substantial health burden at the population level. Marshall says the “conservative” estimate is that about 10 percent of survivors develop Long COVID. He thinks the rate is likely closer to 30 percent, but some studies place it even higher. With more than 78 million confirmed infections in the U.S. since early 2020, that means potentially 25 million or more Americans have had PASC at some point.
That’s why the NIH needs a broad network to conduct RECOVER. UMMC is one spoke in a larger study hub of participating institutions led by West Virginia University. The Medical Center is a critical location because it serves a high proportion of people who appear to be most at-risk for Long COVID. Black Americans experience PASC at a rate nearly three times higher than white Americans. Marshall says PASC also appears more frequently in rural residents.
Amy Wigglesworth, a clinical research nurse working on RECOVER, said UMMC started recruiting participants in December 2021. They aim to enroll about 83 adults in the study by May.
After reviewing eligibility and completing an informed consent process, Wigglesworth said participants will undergo some procedures similar to a regular doctor’s visit, like measurements of their blood pressure, height, weight and blood work. They may also give additional samples of blood, nasal swabs or other body products to make part of the study’s biorepository.
In addition, participants will fill out an extensive questionnaire about their health history pre- and post-COVID.
“Based on the answers participants give, we may flag them for a follow-up procedure, such as a CT scan or pulmonary testing,” Wigglesworth said.
RECOVER will follow its participants for four years, including additional clinic visits and phone calls.
While the study primarily needs participants who have been diagnosed with COVID-19, Wigglesworth said RECOVER requires healthy volunteers as well.
“We’ll also recruit some individuals who haven’t had COVID-19 as controls,” she said.
Studying Long COVID is important because it gets at a sometimes-overlooked dimension of the pandemic: that the potential outcome of a SARS-CoV-2 infection aren’t simply live or die. Millions of Americans have experienced temporary – or perhaps permanent – disabilities that affect their ability to live as they used to, all due to COVID-19.
And with hundreds of new cases diagnosed daily in Mississippi, COVID isn’t going away anytime soon, Marshall said.
“Even though we may be seeing some light at the end of the tunnel, there are other viruses that will come,” Marshall said.
For more information about the study, visit https://recovercovid.org/.


