Eye care providers can often spot the unexpected during routine exams
When a third-grader has trouble seeing the board at school, a routine visit to the eye doctor likely will end with a new pair of glasses.
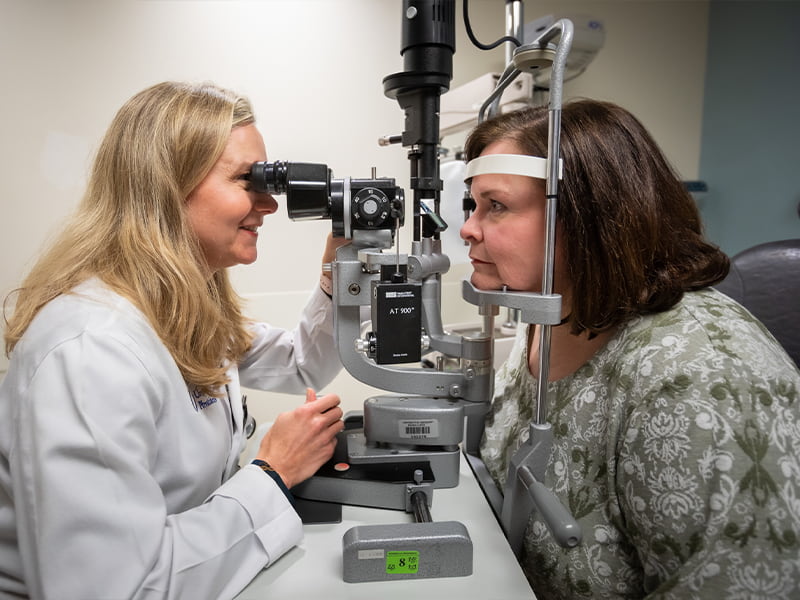
For Ridgeland resident Grace Thaggard, however, the appointment revealed something much more life-changing. Dr. Kimberly Crowder, now chair of the Department of Ophthalmology at the University of Mississippi Medical Center, saw significant inflammation that immediately concerned her.
“Dr. Crowder pulled my mom aside and said, ‘I see something, and it’s worth checking out,’” said Thaggard, now a 21-year-old chemistry major at the University of Alabama-Birmingham

Crowder referred Grace to pediatric ophthalmologist Dr. Nils Mungan, a professor in the Department of Ophthalmology. The diagnosis: Grace was positive for HLA-B27, a protein on the surface of white blood cells that places you at a higher than average risk for autoimmune diseases such as inflammation of the bones of the spine and arthritis.
Grace also was diagnosed with bilateral iritis, a swelling and inflammation in the colored ring around the pupil of the eye. That condition is often found in people who develop certain autoimmune diseases that have a possible genetic association.
A blood test pinpointed Grace’s HLA-B27, which can be genetically passed down. “I wondered if it had come from me,” said Grace’s mom, Carol Thaggard. “I knew I had something rheumatological.”
Grace’s father and Carol Thaggard’s husband, Dr. Anson Thaggard, is an associate professor in UMMC’s Department of Radiology.
Carol Thaggard was being treated by Dr. Vikas Majithia, UMMC division chief of rheumatology, for the autoimmune disorder mixed connective tissue disease. “He tested me, and I had HLA-B27,” she said. Years later, Crowder diagnosed her with iritis.
Other than the inflammation that she never felt, Grace had no symptoms when Crowder first examined her. HLA-B27 is just one example of conditions that an ophthalmologist or optometrist can detect or suspect from a routine eye exam, Crowder said.
“I don’t think that I will ever stop being amazed that I find the unexpected on eye exams,” Crowder said.
Patients can learn for the first time they have one of an array of conditions or diseases – diabetes being a frequent one - thanks to an eye exam. High blood pressure, autoimmune diseases, sexually transmitted diseases and some cancers are among conditions that can come to light during an exam, in addition to warning signs that a patient may be at high risk for stroke.
The eye is the only place in the body where a doctor has an unobstructed view of blood vessels, nerves and connecting tissue without performing surgery. They use special instruments and powerful lenses to examine the front and the back of the eye, looking carefully for conditions that can affect each of those areas.
It’s why the American Academy of Ophthalmology on its website calls an eye exam “a window to our soul and body’s overall health.”

Dr. Roya Attar, an optometrist and assistant professor of ophthalmology, remembers examining a healthy patient who was experiencing vision changes. As Attar peered into the woman’s fundus, or the back part of the eye, “I noted that she had a unique bleeding pattern in her eye,” Attar said. Retinal hemorrhages with a white center, known as Roth spots, are relatively rare.
Concerned, Attar referred her patient to UMMC retinal specialist Dr. Brian Tieu, assistant professor of ophthalmology. Following that retinal consult and a medical workup, the patient was diagnosed with multiple myeloma, a serious blood cancer. Because the eye exam resulted in the cancer being discovered early, Attar said, “her survival rate improved dramatically.”
In many cases, patients don’t seek out an eye professional unless they’ve noticed a change in their vision or have significant eye irritation or pain, Attar and Crowder say. “And unfortunately, the majority of patients don’t have regular annual eye exams, despite the universal sentiment that sight is our most treasured sense,” Attar said.
Patients also may not realize that blurred vision, eye irritation and redness can’t always be remedied by glasses or over-the-counter eye drops, Attar said. They can be clues that a patient has a far more serious eye or other health condition, such as diabetes, one of the most common causes of blindness worldwide. Diabetic retinopathy, a complication of diabetes, is the top retinal vascular disease.
Signs a patient could have diabetes include sudden shifts in a patient’s eyeglasses prescription or sudden blurred distance vision. Attar advises such patients to see their primary care physician for an evaluation of their blood sugar and other diabetic markers before their eye care provider prescribes glasses.
In Grace Thaggard’s case, the partnership between Department of Ophthalmology providers and those in other Medical Center specialties was critical to her treatment, which continues today. Grace also saw Majithia, who placed her on medications to control the autoimmune issues associated with HLA-B27.
Make no mistake: An eye exam should never replace the need for patients to regularly see their primary care provider, Crowder said. “I am not a primary care doctor, and I will never have that knowledge and expertise without going back to repeat residency training,” she said.
If Mississippi is going to make an impact on chronic diseases like obesity and diabetes that place the state “in the top 10 on all the wrong lists,” Crowder said, primary and population health programs must vastly improve.
“If I’m diagnosing diabetes in an adult, then the system is very broken, because once I see diabetes in the eyes, the patient has had the disease undiagnosed for quite some time,” she said. “The focus has to be shifted to prevention. I agree with appropriate referrals to eye doctors for many disease processes, but it upsets me to see the current system is failing our population.
“The answer is not, and never will be, ‘Get more eye exams.’”
Her parents’ diligence in ensuring she get good eye care, however, made all the difference for Grace.
Being diagnosed in elementary school “was a lot,” she said. “Your main fear as a third-grader is going blind. It was overwhelming at first, but I knew that if it had been untreated, you could have degenerative effects.”
She managed her condition with steroid drops until they eventually caused problems with the pressure in her eyes. On her current medications from Majithia, “I haven’t had a flare-up in three years, and I haven’t had to use the drops.”
A UAB junior, Grace is studying German and forensic science in addition to chemistry, with plans to pursue her doctorate in inorganic or environmental chemistry.
“The good news is it doesn’t hurt,” she said of her condition. “The bad news is that my body isn’t going to give me warning that something is wrong. That’s why I go to the eye doctor every six months and have bloodwork.
“But had I not had problems seeing the board as a third-grader, I don’t know when we would have figured this out. The main problem had nothing to do with my eyes.”


