No falling down on the job: Patient care team garners safety award
When a patient hits his buzzer on University Hospital's 5 North, a staff member dedicated to answering calls for help bustles to his bedside.
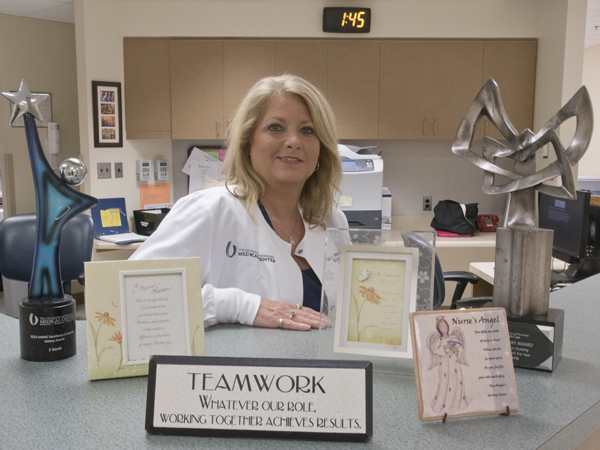
It's just one facet of a program instituted in September 2014 by 5 North nurse manager Cissy Bailey as she collected data for a project requirement in her quest to earn a doctor of nursing practice degree. Her mission: Gather information on when patients fall the most and why, and come up with a solution.
"When I checked the data that I was collecting, I saw that a very high percentage of patient falls happen between 11 p.m. and 7 a.m., with a peak time of 4 a.m.," Bailey said. "I thought, why is this?"
Bailey instituted a program in which her nursing team increased the "rounding," or nurse visits to patient rooms. And, she went a step further, pulling one person from that shift and dedicating them to immediately responding to patients who call for assistance.
"When a patient falls, immediate assistance is needed," Bailey said. "When the call light rings, the assistant pulled from staffing doesn't wait to be notified. They immediately respond to that patient's need. Otherwise, the person might not wait for help, get up without assistance, and fall."

Her team's aggressive effort to stop patient falls before they happen is getting national notice. UMMC is one of only two hospital systems in the country awarded a 2015 Stand Up for Patient Safety Management Award from the National Patient Safety Foundation. New York-based North Shore/LIJ Heath System is receiving the same award, in its case for developing a system-wide effort to ensure accurate patient identification.
Bailey's nursing team changed its approach, adding patient care technicians and nursing assistants to those performing both routine and variable rounds, with variable visits occurring more frequently. During the last four months of 2014, the rate of falls on the unit declined from 6.2 falls per 1,000 patient days to 1.19 falls per 1,000 patient days.
Falls are classified under hospital-acquired conditions (HACs), or reasonably preventable conditions that patients didn't have upon admission, but instead occurred during their stay. It's an area in which the federal Centers for Medicare and Medicaid Services has cracked down, levying financial penalties in December to more than 700 hospitals nationwide, including UMMC.
Bailey found that patients tended to fall more in the predawn hours because their sleep is disrupted by routine care activities in their rooms - for example, vital signs are scheduled to be checked at 4 a.m. "That was our ah-ha moment," Bailey said.
"The patient wakes up, and they're groggy," Bailey said. "They think they can get up by themselves, and they don't call for help. They get up and they fall. People often overestimate their ability to walk alone."
Her nursing team is averting that by rounding more frequently and answering buzzers as soon as they sound. "It immediately started making a difference," Bailey said of the new approach.
When Medical Center nurses round by a room, they assess the chance of a fall by checking the four Ps: personal items, potty, pain and positioning. That can involve making sure the most direct path from a patient's bed to the bathroom is free from obstructions or slip hazards, and making sure a patient's personal items such as glasses or cell phone are within easy reach.
"We have found that patients are now more likely to wait for the rounder than try to get up by themselves, knowing how frequently the rounders visit and how quickly they respond," Bailey said.
Fall prevention remains a top concern at UMMC, where the 900-plus nurses dedicated to adult patients take a variety of precautions to keep them out of harm's way. That includes assessing all patients for fall risk when they are admitted, posting signs in their rooms urging them to ask for help, and making their families part of that conversation.

In early March, nurses began using a falls prevention care plan developed and validated at the University of Arkansas for Medical Sciences. A nurse details patient information such as age, physical or mental disabilities, or medications that can cause confusion or dizziness to produce an individualized care plan for the patient that predicts the chance of falls.
UMMC's patient safety officer, Amber Arnold, led the Medical Center's March 8-14 observance of National Patient Safety Awareness Week. It focuses on the relationship between medical staff, patients and patient families, and encouraging health-care providers to include patients and families in their own care to better keep the patient from suffering harm such as falls.
The Stand Up for Patient Safety Management Awards will be presented at the annual NPSF Patient Safety Congress April 29-May 1 in Austin, Texas.
"One of the best parts of our annual meeting is the opportunity to publicly recognize these important initiatives," said Tejal K. Gandhi, the foundation's president and CEO. "Members of the Stand Up for Patient Safety program at NPSF are leading the way in patient safety, and we are pleased to be able to celebrate successful efforts such as these."
Bailey hopes that dedicating a staffer to answering patients' buzzers can be initiated on other Medical Center hospital floors. "When I would have more falls, it seemed to be most frequent when I had to pull that (designated) person back into staffing because we were short-staffed. That one extra person can make a big difference."
Bailey said she's humbled to receive the award on behalf of 5 North staff and the Medical Center.
"The success of this project is due to all the support and dedication of all involved," she said. "I by no means made this journey alone.


