STORK training critical when lives of moms, babies in jeopardy

In his four and a half years as an emergency medical technician with a rural ambulance service, Zachary Jackson has delivered just one baby – a full-term, healthy little one whose mom did just fine.
He hasn’t been that emergency responder who arrives at a rural residence, or perhaps on the side of a road or highway, to deliver a preemie, especially one as early as 24 weeks. He hasn’t tried to give care to a mom who is hemorrhaging following a birth, or whose blood pressure shoots dangerously high or low.
“I’ve been lucky,” said Jackson, a rural Neshoba County resident who’s training to become a paramedic.

But in a state like Mississippi, where infant and maternal mortality ranks among the highest in the country, emergency responders, nurses and providers in small, rural hospitals often must deliver pre-term babies and work to save the lives of mothers who can experience a plethora of life-threatening complications before and after giving birth.
They need the tools to stabilize a mom or baby in trouble – to keep them alive – until they are transported to a higher level of care. The University of Mississippi Medical Center is making that happen by taking hands-on training directly to those who need it the most.

“Emergencies occur every day in obstetrics. No one wants to do that emergency delivery, whether it’s normal, preterm or breech. It can be terrifying,” said Dr. Rachael Morris, UMMC associate professor of obstetrics and gynecology.
“We have a long, skinny state, and not every area that sees patients has the benefit of having an obstetrician on staff. In a lot of areas, providers are doing a great job, but they haven’t had formal obstetrical and gynecological training.”
Morris and a team of UMMC providers are blanketing the state with both classroom-style instruction and real-life scenarios using sophisticated simulation moms and babies who talk, cry, scream, breathe and register vital signs such as heartbeat and rate of respiration.
The training is called STORK, which stands for Stabilizing OB and Neonatal Patients, Training for OB/Neonatal Emergencies, Outcome Improvements, Resource Sharing, and Kind Care for Vulnerable Families. UMMC’s Mississippi Center for Emergency Services is using a grant from the W.K. Kellogg Foundation to carry out STORK.
“A lot of people think a rural ER is a Band-Aid station, and you don’t need to know much. The opposite is true,” said Kacey Jones, a nurse practitioner at Lackey Memorial Hospital in Forest.
“It’s no surprise that over the last several decades, maternal mortality across the country and in Mississippi continues to be a huge problem,” Morris said. “The culprits for mortality and morbidity remain the same: hypertensive disorders and hemorrhaging, and in Mississippi, a huge problem with preterm deliveries.”
The infant mortality rate in Mississippi- 8.3 deaths per 1,000 live births in 2020 – is the nation’s highest. Ditto for preterm births, 14.19 per 1,000 live births, most recent statistics from the Centers for Disease Control and Prevention show.

On July 27, Morris and team traveled to Lackey Memorial to train emergency room staff from that hospital in addition to several from Magee General Hospital. The team also includes Dr. Tara Lewis, an assistant professor of emergency medicine, and Emily Wells, a nurse practitioner with UMMC’s neonatal and pediatric transports. UMMC has the state’s only children’s hospital and only Level IV neonatal intensive care, the highest designation.
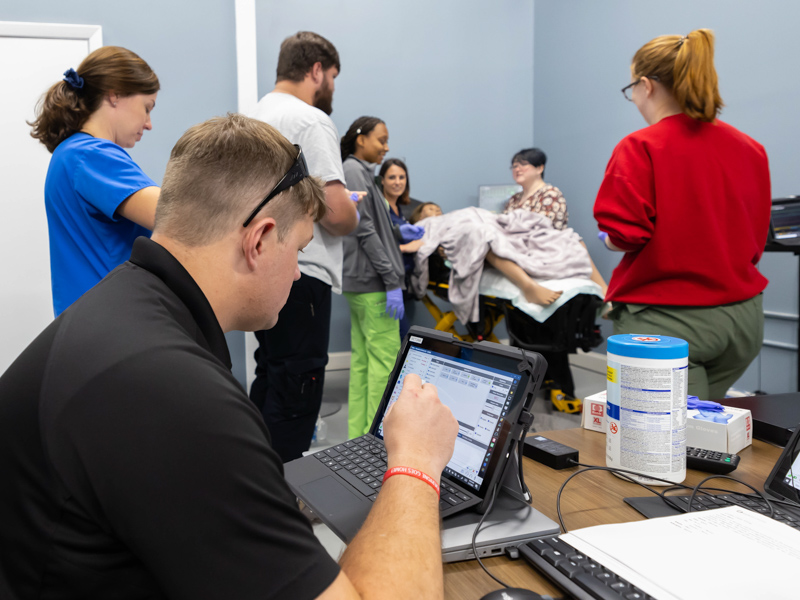
Also on hand was Will Appleby, a critical care transport educator with MCES and “our technical software mastermind” who facilitates scheduling of training and logistics, Morris said.
Their overarching message: If you don’t treat the mother, then the baby’s chances of making it takes a nosedive.
Case in point is high blood pressure. A mom “can have very mild symptoms that might escape a regular provider unless they have a sense of awareness in the forefront of their mind that it can be life-threatening,” Morris said.
A blood pressure of 140 over 90 in a pregnant mother can be very alarming, but in a 45-year-old man, is not big deal for the most part. Pregnancy-specific diseases can create terrible outcomes if you don’t recognize what’s happening, and triage and treat it appropriately.”
If a woman is bleeding after a delivery, Morris said, “it’s absolutely life-threatening. You can lose your entire blood volume in minutes. Knowing how to use certain medications and how to perform uterine massage are small key elements that help to save lives.”

Morris and the team demonstrated just how much blood a mom can lose during and after delivery by filling a basin with a red liquid, plus soaking a two-foot by two-foot pad in red liquid, and comparing it to a pad the side of a small baby’s diaper.
“If you’re not ready for a hemorrhage at delivery, you’re already behind,” she told the emergency room staff. “I can’t tell you how important it is to know how much blood a mother has lost. She can tolerate it until she’s about to die.”
They’re just two of many emergencies providers will see – often – in rural areas where they may have too little education, and not enough confidence in the moment, to save or stabilize moms when the clock is ticking.
“You need every bit of cardiac output to be pregnant and go into delivery,” Morris said. “It’s like running a marathon. Right after delivery is peak time for pulmonary edema (excess fluid in the lungs). If you’re not ready for it, you can be in trouble.”
Lackey Memorial doesn’t have a true operating room, and its emergency room is small. “It’s staffed by a nurse practitioner or an emergency room doctor – one or the other- and our nurse,” Jones said.
Moms in rural areas go into preterm labor “frequently,” said Hayden Neal, a registered nurse who works both in Lackey’s ER and UMMC’s surgical intensive care unit. They often had no prenatal care, and “a lot of times, they don’t know how many weeks they are. We treat to what they came in for, and then we transfer them to Wiser (the UMMC hospital for women’s OB-GYN care).
“That’s our biggest thing – no OB care,” Neal said. “They have to go to Meridian or Jackson. That’s an hour. A lot of people don’t have transportation.”
The team led Jackson and a dozen-plus Lackey ER providers through simulations using Victoria, a mother in labor, and Tory, her newborn baby. “Make it real. Put your gloves on,” Morris told them. “It’s really, really cool.”

Morris was dead serious as she laid out the scenario. As simulator Victoria screamed, “The baby is coming!” Morris quickly said: “Mother is 39 weeks. She’s advanced maternal age, over 35. She’s three centimeters dilated and feels the urge to push. She had a prior uncomplicated vaginal delivery.”
Victoria screams, a lot. “How often are you having contractions?” Morris asked her as the ER staff gathered close to the bed. “Every one to three minutes,” Victoria answered.
“She’s going to deliver. We need to be ready,” Wells said. “I’m going to call for pediatric transport just to be ready.”
The baby’s head emerged. “Once the head comes out, don’t be afraid,” Morris said. Then, Lewis demonstrated how to ease out the baby’s shoulders, then grab the baby behind the neck. “Now, lift the baby straight up. It can be difficult to pull the baby out,” Lewis said.
Don’t assume this mom was delivering in the hospital. “When we go to the rural areas, nine times out of 10, the babies have been delivered at home,” Wells said. “We have tons of premature babies delivered at home. We go to pick them up, and they’re cold.”
Three of the Lackey ED staff take Victoria’s full-term baby to an isolette for instruction from Wells. Kristen Robinson, a registered nurse in Lackey’s ER, gently massages her back and suctions her nose and mouth. She’s doing well.
But Victoria might not be in the clear. It’s potentially a dangerous time during the birthing process. “If there’s no bleeding and no big tear, you’re probably home free. But if there’s bleeding, you’re not,” Morris advised.

Give a bleeding mom the drug Pitocin, which causes the uterus to contract to shut down the bleeding, Morris said. “Zach, if she’s hemorrhaging, your truck should have Pitocin,” she said. “Once that baby is out, give it to her in each thigh. That’s the first drug we should use.”
Victoria did well. But in scenarios where the baby was delivered breech or was preterm, there was considerably more stress and danger to mom and baby.
Victoria groaned as she prepared to deliver a baby that’s breech, or backside first. “Do you see the butt? Everybody feel it,” Morris told the ER staff. “That’s a foot. That’s a hip. We’re going to call for the NICU team because this baby’s going to be very stunned.”
“Even for skilled providers in the NICU, it can make you a little more nervous to intubate a smaller baby. You have to be more precise and deliberate with your skills,” Wells said. “I can’t imagine how much more intimidating it can be for EMS responders than for us.”
STORK training saves lives.
“When you don’t see a lot of pregnant women and then one walks in your door, you have to rely on the training you have. Any increase in training will help you improve outcomes,” said Lewis, a labor and delivery nurse before going to medical school.
Because interest is so widespread, MCES plans also to offer quarterly training at UMMC for any Mississippi providers or emergency responders who would like to attend.
“This is probably one of the most impactful and exciting things that I’ve been able to be a part of,” Morris said. “I’m so fortunate that they asked me to do this. This definitely ranks at the top of things I feel will make a difference.”


