Study urges careful use of kidney calculations
New research from the University of Mississippi Medical Center shows that the two main methods of assessing kidney function provide substantially different results in about half of patients, which could lead to missed opportunities to prevent or manage renal disease.
The paper, published online July 5 in the Annals of Internal Medicine, focuses on glomerular filtration rate (GFR), which refers to the amount of fluid the kidneys filter per minute.
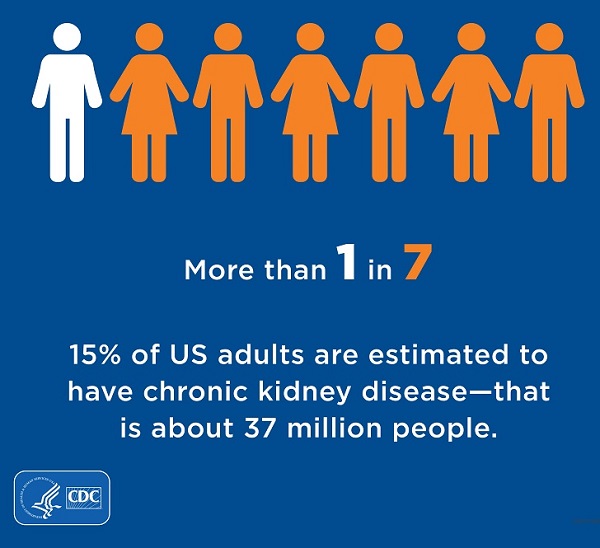
About one in seven U.S. adults have chronic kidney disease (CKD). Left unmanaged, CKD can progress to kidney failure, which requires dialysis or a transplant. More than 500,000 Americans live with this “devastating” condition, said Dr. Tariq Shafi, professor of medicine and John D. Bower Chair of Nephology at UMMC.
“We want to prevent that from happening and prevent the progression of kidney disease,” said Shafi, co-lead author of the study.
Diagnosing CKD and determining its severity is a critical part of getting patients the treatment they need. Doctors use GFR to do this. A GFR above 90 is considered healthy function, between 60 and 89 could be a sign of early CKD, between 15 and 59 is moderate to severe CKD, and under 15 is kidney failure.
In most cases, doctors use equations and the patient’s serum creatinine levels or cystatin C levels to calculate an estimated GFR, or eGFR, to make decision about further testing and treatment.
The problem is that “estimated GFR is not an absolute or direct measure of kidney function,” Shafi said.

For that, doctors need to use directly measured GFR, or mGFR. However, “This process is not feasible for every patient,” said Dr. Xiaoqian Zhu, a postdoctoral fellow at The MIND Center and the study’s other lead author.
The central question for the research team, Shafi said, was “What is the likely range of directly measured GFR for a patient with a given eGFR calculation?”
If that range is narrow, then a patient’s eGFR is likely reliable. If wide, it is possible that using eGFR alone to assess kidney function could lead to a misdiagnosis.
The study used data from 3,223 people enrolled in four cohort studies focused on cardiovascular or kidney diseases. One of those, the Genetic Epidemiology Network of Arteriopathy (GENOA), includes participants from Jackson, Miss. The researchers determined eGFR and mGFR for each participant and used them to find a range of potential mGFRs at the different eGFR levels.
“Our key finding in this paper is that the range of mGFR at each eGFR is actually quite wide. As a result, you really need to see eGFR reported with its range to avoid its misinterpretation.”
For instance, at an eGFR of 60, the threshold for defining CKD, Shafi and colleagues found that 95 percent of people could expect to have an mGFR between 36 and 87. This spans from the severe stage 3b CKD to normal kidney function.
They also found that eGFR and mGFR agreed on the stage of CKD only about the half the time. For example, in their group with an eGFR of 30 to 44, or stage 3b CKD, 53 percent of participants had an mGFR that was also between 30 and 44. Meanwhile, 35 percent had higher mGFRs consistent with either stage 3a CKD or only mild dysfunction, while 12 percent had mGFR associated with more severe stage 4 CKD.
“Uncertainty in eGFR is well-recognized but not fully appreciated, and we wanted to quantify that uncertainty,” said Zhu, who conducted this research as part of the PhD in biostatistics and data science she earned this year from the John D. Bower School of Population Health.
While eGFR alone may not provide reliable findings for individual patients, it is useful at the population level.
“Estimated GFR helps identify the groups of people who are most at-risk for complications of kidney disease. It is an excellent population health tool in that regard,” Shafi said, likening it to an average. “The problem is that few of the patients are average.”
Shafi thinks there is a risk that physicians are “lulled into safety with eGFR, thinking that eGFR is exactly the same as directly measured GFR and then base clinical decisions based on this misinterpretation,” he said.
These findings highlight the need to make direct GFR measurements available to patients who need them, Shafi said.
However, he says there are challenges to getting an mGFR. One method requires nuclear imaging techniques, and “we don’t want to unnecessarily expose people to radiation,” he said. Another approach uses non-radiolabeled dyes, but it lacks a medical billing code limiting its use.
Shafi says that using mGFR should be made available for clinical care, particularly for those using certain chemotherapy drugs or planning to donate a kidney. Last year, UMMC started directly measuring GFR for all living donors as part of the routine living donor evaluation process.
As a nephrologist, Shafi said it is his charge to figure out how to deliver the appropriate kidney care for each patient.
“Not everyone needs to get a direct mGFR measurement. But it should be available when we need it.”
The National Institute of Diabetes and Digestive and Kidney Diseases funded the research studies that collected the data used for this paper. Additional study authors represent the Mayo Clinic, Johns Hopkins University and Baylor Scott and White Research Institute.


