For sickest patients with COVID, struggle for recovery begins with emergency care

Dr. Kendall McKenzie can quickly describe what he finds most daunting about leading an Adult Emergency Department brimming with patients with COVID-19.
“The most challenging days so far, and what I also project that is not going to end any time soon, are the days where all of our designated COVID rooms are occupied, and additional patients who are either known positive or unknown come in,” said McKenzie, chair of Emergency Medicine at the University of Mississippi Medical Center.
“You have the logistical challenge of finding a space to start treating those patients. Those are the most anxiety-provoking times,” he said. “You want to limit that person’s exposure to patients and employees, and to be as safe as possible, but there are physical limitations when we are so full.
“You have to survey the scene and figure out, in the moment, what changes you will make – where you will put patients, and how you will take care of them.”
Most days, the Adult ED is full and then some. Of the 52 total beds, 11 are reserved solely for confirmed or suspected patients with COVID. The overflow patients are cared for in 12 acute care beds.
The overflow after that go anywhere there’s room. And on any given day, 15 of those 52 beds – on some days, 30-plus beds – are taken up by patients, COVID or not, who are waiting hours or even a day or two for a bed in a hospital that stays at capacity. That greatly impacts the availability of beds for ED patients still waiting for treatment.
That crush means some very sick patients seeking UMMC’s specialized care must be treated somewhere else, and that might be out of state. “When you have no beds and we’re holding patients in the ED, your system can only take so much,” McKenzie said.

Some of the very sickest patients with COVID need to be on a ventilator. “They are way behind the eight ball,” said Laura Watrous, a registered nurse and nurse educator for the 100-plus providers and support staff in the Emergency Department.
“We can get them intubated, but they are so sick. The virus is throughout their body.”
As the pandemic rages, hundreds seek care every day at UMMC’s Adult and Pediatric EDs and at Women’s Urgent
Care primarily for obstetric emergencies.
Some patients with COVID are more scared than acutely ill. Others are in much worse shape than they know.
“The trend is that the patients with COVID coming to us now are sicker than the ones who would come to us three months ago,” said Executive Vice Chair of Emergency Medicine Dr. Risa Moriarity.
“We tend now to see patients who were tested maybe a week or two earlier and were positive,” Moriarity said. “Either they, or in consultation with their primary care physician, made the decision to stay home, which was appropriate at the time, but their symptoms have worsened.”
The inability to take in oxygen is what drives most patients with COVID to an ED.
“Most patients don’t have a home oximeter. They don’t know that their oxygen level is dropping, and you can have a really low oxygen saturation level and still be mentally alert and hold a conversation,” Moriarity said. “That’s pretty unique to this disease.”
And although many who do or might have the virus are treated and sent home, inpatient numbers for confirmed and suspected cases have been running in the mid- to high 90s, reaching at or near 110 on some days during the past several weeks. That’s in addition to patients with COVID who reach the stage of convalescing, but not ready to go home.
“We’ve had some come in who are end of life,” Watrous said. “And then we have patients with COVID in the ED with a lot of comorbidities. You might think they aren’t going to make it, and they get discharged from the hospital.”
Extremely ill patients with COVID also are seen at Women’s Urgent Care, a 24/7 operation housed in Wiser Hospital for Women and Infants. “We have unfortunately had some pregnant moms sick enough for the ICU,” said Yolanda Moore, Women’s Urgent Care nurse manager.
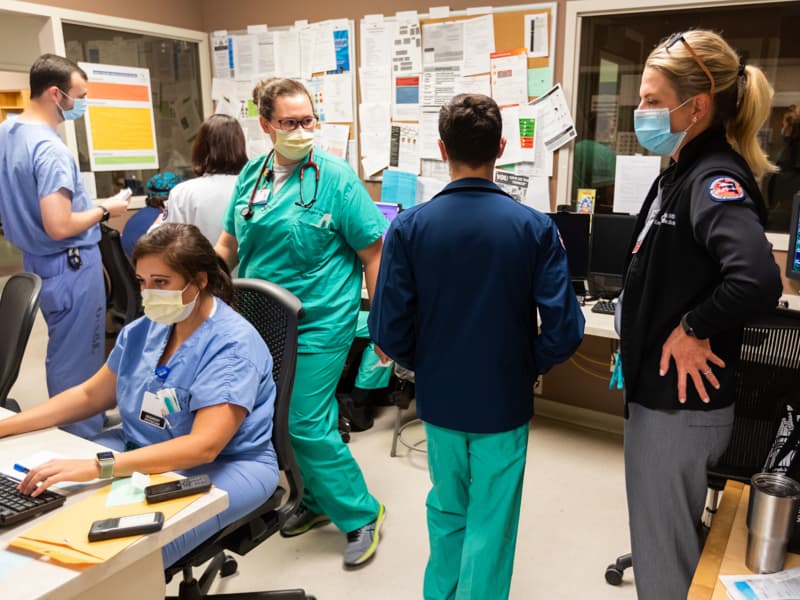
Emergency medicine is stressful, global pandemic or not. UMMC’s emergency medicine physicians, nurses and support staff are meeting the new challenges to care wrought by the virus.

Not sure if an unresponsive trauma patient is COVID-positive? There’s a plan to find out.
The number of patients over ED capacity triples over a couple of hours? There’s a plan.
What if a tornado slams a Mississippi town? And the ED is full of patients with COVID?
There’s a plan for that, too.
“The staff is tired. They are fatigued,” Watrous said. “We don’t get a break from it. We came to work when the rest of the world was sheltering in place.
“But, we love doing this, because we love what we do.”
*
When a patient arrives at the Adult or Pediatric ED or Women’s Urgent Care, you assume they could be COVID-positive. If they’re going to be admitted, they’re tested; otherwise their provider makes a call depending on symptoms or other available information.
“You will have a trauma patient from a car wreck, and they’ll turn into a patient with COVID. If a patient with an altered mental state comes in and can’t answer questions, we’ve had to treat them as positive unless we know otherwise,” Watrous said.

Most Adult ED exam rooms are now isolation rooms. Patients check in at a tent by the ambulance bays. They’re screened for COVID, and if they already know they are positive or have symptoms, they go straight to isolation.
Nurses question ambulance paramedics about their patient’s COVID status. “If we don’t know, we don’t take any chances,” Watrous said.
On a recent day, a patient from a metro-area nursing home came in by ambulance. They’d tested positive several weeks earlier and were thought to be recovering, but developed fever and other symptoms. That person went to isolation.
The staff awaited several transfers from nursing homes. At the same time, a rolling electronic board managed by MED-COM, the state’s emergency communications clearinghouse operated by UMMC, showed patients en route and descriptions of their traumatic injuries.
“When someone is transferred to us, we might be told that they are looking good,” Watrous said of patients with COVID. “It can rapidly change.”

“Although we’re seeing a lot of patients with the same disease, and that has never really happened historically in our ED, in some ways this is business as usual,” Moriarity said. “We get patients every day and we look at them and say, ‘This person needs to be immediately intubated. This person needs immediate resuscitation.’”
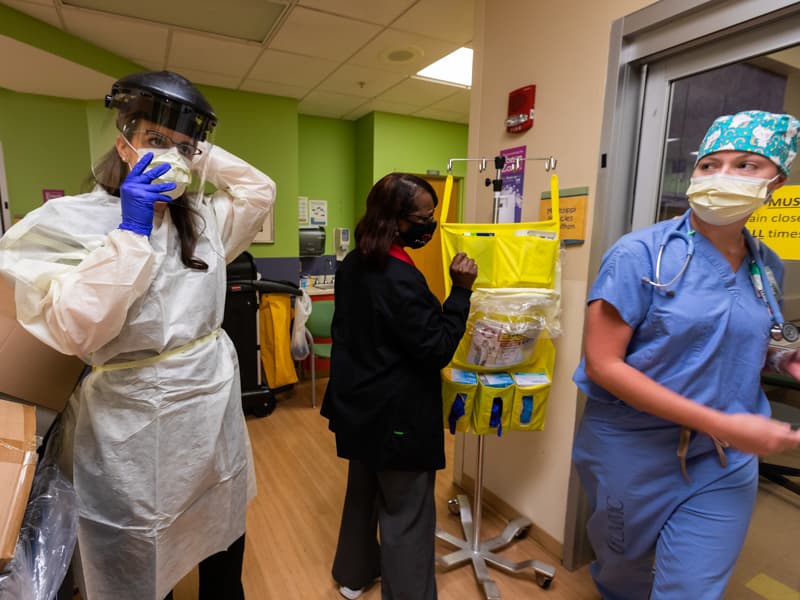
Care for patients with COVID often seems a continuous motion, with many hands working after their owners quickly don personal protective equipment: yellow gowns, blue gloves, a face shield. They’re already wearing a face mask.
Such patients “are a lot more time-consuming,” Watrous said.
Moriarity recalls recently sitting at her computer in the ED and seeing paramedics roll a patient with suspected COVID past her. “I could tell the patient was really working to breathe,” she said.
After a quick discussion with the charge nurse, Moriarity said, she put on PPE, gathered the equipment needed to intubate the patient and entered his room, where EMTs were stabilizing him.
“In a non-COVID situation, there wouldn’t be that slight delay,” she said.
*
So far, UMMC’s Pediatric ED isn’t besieged by COVID. As of August 5, caregivers had tested about 2,363 children. Of that number, 173, or about 7.3 percent, were positive. Children also get tested in a nearby pediatric acute respiratory care clinic.
Twenty-one, or less than 1 percent, had been admitted as of August 5. None have died.

Dr. Benji Dillard hopes those numbers don’t significantly worsen.
“With school starting back, we expect to see an uptick, but also an uptick in other things we see in the fall, like strep and flu,” said Dillard, division chief of pediatric emergency medicine. “Absolutely, kids can get COVID. Absolutely, kids can transmit COVID. Those are just the facts.
“They are getting it with more frequency now,” he said. “And, they could have COVID and strep, or COVID and flu. One germ doesn’t always stand alone.”
Patients with one or more symptoms are isolated and often get a swab stuck up each nostril. That’s a reason why all of the Pediatric ED’s 26 exam rooms are outfitted with HEPA filters that force air through a fine mesh that catches airborne coronavirus particles.
“Some parents are actually refusing the test,” Dillard said. “They say they don’t want their child to have to go through it. If they refuse to let their child be tested, we tell them to go home, isolate, and treat it as if they have COVID.”

Women’s Urgent Care and UMMC’s maternal-fetal medicine specialists see many of the same patients. As of August 4, caregivers had seen 106 patients who were positive for COVID, and from that group, logged 68 deliveries.
Sometimes, patients who are COVID-positive are seen at Women’s Urgent Care are hospitalized, either on Wiser’s Labor and Delivery floor, or on a University Hospital floor reserved for patients with COVID, Moore said.
Pregnant COVID-positive women now receive care not in UMMC’s obstetrics and gynecology clinics, but instead through telehealth or visits to Women’s Urgent Care. “It’s very strategic, individualized care,” Moore said. “If they come to Women’s Urgent Care, we have staff ready to receive them and take them straight to an isolation room.
“Over the last two weeks, we’ve definitely seen a growth in these patients. From mid-May until now, we’ve seen about 95 patients with suspected COVID.”
*
The EDs are used to treating all comers. “That’s an underlying philosophy of this institution,” McKenzie said. “That’s why it’s so uncomfortable to tell a physician, ‘We can’t take your patient.’ You can only have a certain critical mass before it becomes a safety issue.
“I fear we are about to learn a lot about this virus when school starts back. Every classroom is like a petri dish,” he said.
McKenzie is a veteran military surgeon. “With battlefield medicine, you put your head down and do the job, and your main focus is the execution of the mission,” he said. “I see health care workers in this institution with the same attitude.
“That brings a level of comfort to what we are doing,” he said. “It’s a rough ride, but people are going to finish this mission.”


