UMMC research breaks funding record

The University of Mississippi Medical Center had a record year for research and sponsored programs funding, receiving $123.5 million from 392 separate grants, awards and contracts during fiscal year 2021.
The fiscal year, which spanned July 1, 2020 to June 30, 2021, smashed the previous records of $85 million from 2011 and 347 awards from 2020.
The FY21 total includes $15.1 million for COVID-19-related research and $11.8 million in pandemic aid funds via the Coronavirus Aid, Relief and Economic Security (CARES) Act.
The majority of the Medical Center’s outside funding comes from federal agencies to support research projects. There are grants to continue the work of major, long-term projects on cardiovascular disease. Others explore new avenues of inquiry, such as the use of cold platelets in trauma medicine, ear development and injuries, and computer-based modeling of hypertension risk. UMMC also received funding for multiple education programs, which enhance student experience and learning.
Dr. Richard Summers, associate vice chancellor for research, said the sheer number of awards last year demonstrates the strength of UMMC’s research community, from established scientists to trainees receiving their first grants.
“The funds are not just sequestered into large grants with one principal investigator. There are lots of individuals putting forth great research ideas,” Summers said.
One of those researchers is Dr. Joshua Speed, assistant professor of physiology and biophysics, who received an R01 grant from the National Institutes of Health to study the role of endothelin-1 in obesity and insulin resistance.
Endothelin-1 is a “small peptide produced in blood vessels,” Speed said. “Its production is increased in obesity, and this increase leads to insulin resistance and dyslipidemia” but researchers are not certain why.
Insulin resistance is a precursor to type 2 diabetes, while dyslipidemia, or high cholesterol, increases the risk of heart disease and stroke. Mississippi’s high rates of obesity and associated diseases make this line of research critical to the state, Speed said.
With the new grant, his laboratory will study how changes that happen in obesity “disrupt the cellular crosstalk, especially in liver tissue, where we also see an increase in fatty acids in obesity.”
Speed is also interested in the effects on muscle, where cell-signaling molecules called adipokines help manage sugar and fat metabolism.
Grants like R01s, which fund a focused project for several years, allow a scientist to establish a research program.
“It sets the foundation for my career,” Speed said. “This funding also pays salaries for research assistants and lets us look at other biological pathways of interest.”
Summers said that while the Medical Center has built a reputation as being “strong in basic science research, we’ve recently raised our profile in clinical and translational research.”
UMMC activated 84 clinical trials in FY21, primarily funded through industry sponsors. Besides trials for cardiovascular diseases, cancers and other conditions, several projects focused on COVID-19-associated antivirals, vaccines, monoclonal antibodies and rapid tests.
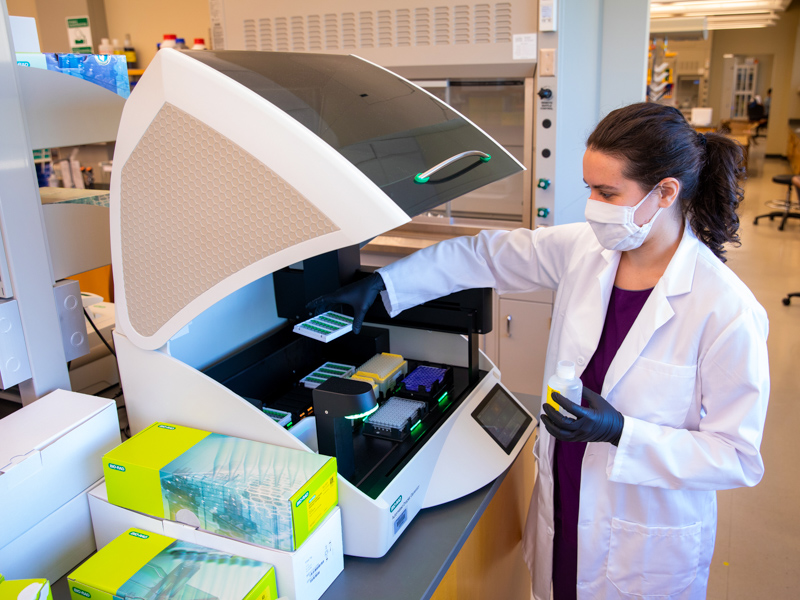
Summers said UMMC still would have had a record funding year without the funds it received for all COVID-19-related research last year. However, the grants and awards the Medical Center received for this work demonstrate the impressive breadth of scientific questions researcher must answer to understand all aspects of the pandemic. Faculty in the Department of Pediatrics received grants to study multisystem inflammatory syndrome in children, a post-COVID-19 complication. The leaders of UMMC’s Molecular Genomics Core Facility received more than $1 million in contracts to track SARS-CoV-2 variantsand fill critical infrastructure gaps needed to manage the pandemic.
“The state and federal officials are calling on us as an academic medical center to do some work that government agencies cannot do,” Summers said. It highlights “the importance of having an academic medical center in our state.”
Meanwhile, Dr. Caroline Compretta, assistant professor of preventive medicine, leads an NIH-funded Community Engagement Alliance Against COVID-19 Disparities project addressing information, vaccination access and clinical trial participation. They received a funding supplement that will help the project continue its work based on the findings from the first year.

“Our listening sessions from the first year informed the ways we developed health messaging for different age groups, and our survey data informed the need for mobile vaccination units,” Compretta said.
The partnership includes the Mississippi State Department of Health, multiple universities, and local groups such as churches and community organizations. Compretta said this multi-stakeholder approach is critical to their success.
“The disease states in COVID-19 are complicated and nuanced, not just in a medical sense but also across ages, races and geography,” she said. Having multiple partner organizations with different skill sets “helps us address the complexities and tailor our responses to each community.”
These kinds of multi-faceted partnerships exist outside of the COVID-19 realm as well. UMMC and MSDH are sharing a three-year, $6 million grant from the Department of Justice to address opioid use disorders through expanded telehealth, naloxone training and coordinated tracking of treatment center beds.

“We want to target everyone in need, from those who are at-risk to those with severe problems,” Dr. Julie Schumacher, professor of psychiatry and human behavior and co-investigator on the award, said last year. “This can help reduce the number of people who fall through the cracks.”
“Even though there has been a lot of focus on the COVID-19, the opioid epidemic will still be present when the pandemic is over,” Summers said. “We expect to see more funding coming for this research next year.”


