Patient falls: First predict, then prevent

Published in News Stories on February 23, 2015
Patients on registered nurse Flora Green's floor have something to look at when they're lying in bed: A sign on the ceiling that tells them not to get up without asking for help, because they could fall.
They may have an alarm on their bed that sounds when they try to leave, sit up, or even roll over, said Green, a nurse educator on the Adult Hospital's 4 North. And, they might have a 4-inch-thick floor mat leading from the side of their bed to the bathroom door, a patient's most-traveled stretch.
They have a nurse's eyes on them at least once an hour as part of patient rounding, and signs posted next to their door alert staff if they're at risk for a fall.
UMMC's 900-plus nurses dedicated to adult patient care take a variety of precautions to prevent falls - and that combination of safeguards is about to get a lot better.
On March 2, Green and her fellow nurses will begin using the Hester Davis Falls Risk Assessment Scale, a falls prevention care plan developed and validated at the University of Arkansas for Medical Sciences. The plan, which integrates with the Medical Center's Epic health record system, is named for Amy Hester and Dees Davis, veteran UAMS nurses who developed it.
Known more simply as the HD Scale, it aims to predict anticipated physiological falls in adult patients in a hospital setting. The program was borne out of UAMS' need to address a previous dismal record on patient falls.
"It's a better assessment tool for those who are a fall risk," Green said. "It will make a big difference in honing in on areas that might not have gotten as much attention through our current system."
How it works: A nurse details, in either an electronic or paper format, patient information such as the person's age, any physical or mental disabilities, or medications that could cause confusion or dizziness. The HD Scale produces an individualized care plan for the patient that predicts the chance of falls. The plan includes interventions, such as bed alarms or signage warning staff the patient is a fall risk, that are tailored to the patient based on his level of risk and additional physiological or environmental factors.
"This is a major step up from the current falls prevention program," said registered nurse Michelle Burns, UMMC nursing workforce specialist and interim director of the Office of Clinical Excellence/Hospital Education.
"We're in a health-care environment where we really need to take advantage of every opportunity to provide better quality of care," she said. "This is a nurse-driven initiative, and nurses are saying, 'We have falls, and we don't like it.' Nurses want to work in a place where they feel safe, and have the equipment and resources to provide good patient care."

Adult Hospital patients have a friendly but firm reminder posted on their room ceiling to view when they're lying down: Don't get out of bed without asking for help, or you might fall.
The new program is one more tool in the tool chest, Burns said. "Nurses are so busy. This is going to help nurses be quicker with their care, more efficient, and give them the resources to provide individualized plans of care and interventions. It will help bring the patient into participating in their own care."
UMMC has been both aggressive and proactive in efforts to lower incidence of falls, with up-and-down success. Falls are classified as hospital-acquired conditions, or reasonably preventable conditions that patients didn't have upon admission, but instead occurred during their stay.
It's an area in which the federal Centers for Medicare and Medicaid Services has cracked down, levying financial penalties in December to more than 700 hospitals nationwide, including UMMC, for patient harm mistakes known as HACs.
Out of a total score of 10, with 10 being the worst, CMS scored UMMC a 10 on serious patient complications, which includes incidences of falls, blood clots and bed sores. That rating was based on two-year-old data and doesn't reflect progress made since then in lowering HACs, including falls.
And, CMS does not reimburse hospitals for injuries resulting from falls, which according to HD is the most common and costly of all adverse events reported in hospitals.
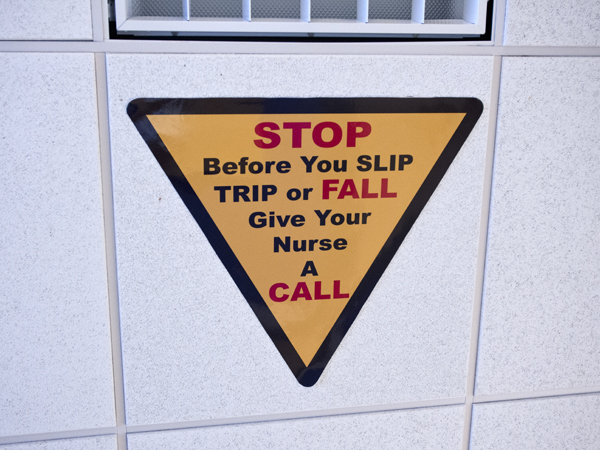
Fall prevention signs posted on the ceiling of all Adult Hospital rooms mean business: Get a nurse's help before you get out of bed.
UMMC's adult hospitals typically average 30 to 40 falls monthly, said registered nurse Keith Hodges, who also serves as director of quality and clinical systems improvement. "The current tool we use just identifies if the patient is at risk or not," he said. "The Hester Davis screen defines not just if the patient is at risk, but why and how, so that we can intervene before a patient falls."
"We've been lucky that over the past four months, we've not had a fall with injury," he said. To be categorized as a fall with injury, the patient must suffer a fracture, dislocation or a wound needing sutures, Hodges said.
Although UMMC has seen a "progressive decline" in the number of falls over the past 12 months, Hodges said, Kevin Cook, CEO of the University Hospitals and Health System, has asked that harm events to all patients be reduced by 50 percent during the current fiscal year.
Hodges, Green and Burns are among about a dozen people on a task force that chose the HD Scale. Because UMMC is very similar in size, number of beds and staff to the University of Arkansas for Medical Sciences, "we think the program will be implemented identically," Hodges said.
Each UMMC adult patient is assessed for individual fall risk, but even then, falls do happen, Green said. If a patient touches the floor, even if the patient says they knelt or slid down, it is documented as a fall, she said.
Green said each time nurses round by a room, they check the four Ps: personal items, potty, pain and positioning.
"Sometimes, a patient is so used to their home setting that when they come in, they don't want to bother the nurse. They don't want to ask for help for such things as assistance with their cell phone from across the room," Green said. "We put those things close to the patients so that they will be less apt to get up, which may lead to a possible fall. I tell my nurses, 'Please get them their glasses. If they can't see, they might fall.' We even place our patients who are at higher risk right near the nurses' station so that they will be watched more frequently."
Patients can sometimes be confused or disoriented, which increases the risk of falling. "A lot of times, patients will not have any family members with them. Just having someone who can sit with them can reduce the patients' chance of falling, because there will be someone who can eyeball what they are doing," Green said.
If a patient falls, Green said, the patient's physician and family are immediately notified. A debriefing takes place where the fall occurred so that floor staff can determine what happened and why, and how it can be prevented in the future, she said.
The task force did its homework before choosing HD. "It is imperative that we implement a program that is proven and backed by research and evidence, that has been trialed, and that has some rigor behind it," Burns said.
In 2011 alone, the HD program saved UAMS $1.27 million in falls-related costs, according to its website, www.hdnursing.com. There's an initial annual licensing fee for hospitals that implement the program, which includes help from HD in getting the program off the ground.
The UMMC task force liked the fact that HD was created by nurses, Burns said.
"That's usually how a problem is solved. Nurses notice a problem in their work area," Burns said. "This program meets our mission of wanting to provide top-notch care."


