Risky business: UMMC, Jackson Heart Study test CVD models
Cardiovascular disease risk models built using majority-white populations also work well for African-Americans, say recent findings from the University of Mississippi Medical Center and the Jackson Heart Study.
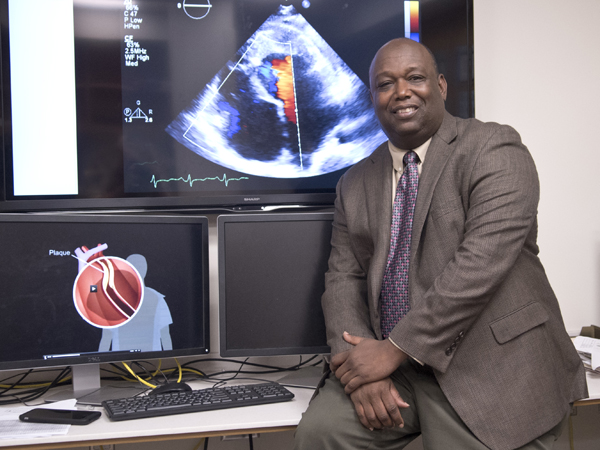
Dr. Ervin Fox, cardiologist, professor of medicine and Jackson Heart Study (JHS) senior investigator, is lead author on the paper, published in the inaugural issue of the Journal of the American Medical Association (JAMA) Cardiology.
"We want to make sure that whatever risk calculator we use applies to an African-American cohort," Fox said.
The Framingham Risk Score (FRS) and newer American College of Cardiology/American Heart Association pooled cohort risk equations (PCEs) are the current standards for determining coronary heart disease (CHD) risk. They include factors such as age, blood pressure, diabetes, cholesterol and smoking.
"Because the Framingham Heart Study was based on a white cohort in a single community, it was not clear whether the FRS would perform as well in estimating the risk of CHD events for patients from other race or ethnicity groups," said Dr. Adolfo Correa, director of the JHS and UMMC professor of medicine.
The PCEs did use data from 4,400 African-Americans, but have never been validated, or tested with, a similar cohort.
Validating the models is important because African-Americans are twice as likely to develop cardiovascular disease (CVD) as whites, Fox says. Underestimating risk could delay or prevent a person from getting the treatment they need, leading to worse health outcomes.
Established in 2000, the Jackson Heart Study aims "to increase our understanding of factors that contribute to the risk and progression of CVD among African-Americans so that prevention interventions can be developed to ameliorate such risks," Correa said. With 5,300 participants, the JHS is the largest study of African-American cardiovascular health in the United States.
Fox and colleagues used the JHS cohort to create their own models that predict risk of CVD events including not only CHD but also stroke and heart failure. They then tested if these models work better than the FRS and PCEs for African-Americans.
"Using statistical models we can tell patients, 'Based on your profile, your ten-year risk of developing cardiovascular disease is this, but if you change certain behaviors, then your risk decreases to this,'" Fox said.
So, how does the doctor predict your chance of a heart attack in the next decade?
Fox and colleagues built risk models using nine years of data from 3,700 JHS participants. They considered variables from three data groups: standard CVD risk factors used by the FRS and PCEs, blood biomarkers and sub-clinical disease variables that describe the heart and circulation.
Fox and team noted which people had a CVD event and determined which variable set best explains who has events and who doesn't. In model building, the goal is to get the most explanation with the fewest variables possible. It's like a tool kit: you would rather build with just a few tools that consistently work well, instead of many unreliable tools that break down.
For example, the JHS data suggests that people who smoke or have type 2 diabetes are about twice as likely to have heart attacks as non-smokers or non-diabetics. Both of these standard risk factors for CVD could, and do, fit in the models.
"We tried to use novel biomarkers that have never been used before (in models)," Fox said.
However, several of the biomarkers didn't predict CVD any better than a coin flip would, so they weren't included.
One notable exception is B-type natriuretic peptide (BNP), which is released by the heart when its walls are stretched too much. High amounts can signal heart failure.
The sub-clinical disease markers, such as left ventricle ejection fraction and hypertrophy (an indicator of how well the heart pumps), were also a new approach to CVD model building.
Among the JHS-based models, the one that included standard risk factors, BNP and the sub-clinical disease variables was the best at predicting CVD. This best model showed slight improvement over the FRS and PCEs for African-Americans.
However, Fox and colleagues conclude that the improvements aren't large enough to make a clinical difference. The older FRS and PCEs "work well in black individuals and are not easily improved on," they wrote, meaning that those models are fine to use.
Why not use the JHS model if it works better, even if only by a small margin?
Using more CVD predictors, particularly LV ejection fraction and hypertrophy, requires an echocardiogram, which is not possible at some resource-strapped clinics.
Also, Fox says that using simpler models allows patients and their physicians to focus on modifiable behaviors such as diet and exercise.
"The model is a strong tool for patients because they can remember their risk when they come home from the doctor's office," Fox said.
However, just knowing your numbers isn't enough to make a difference. You need a change of heart to change your health.
"Patients cannot change their behaviors for only two or three days before a doctor's appointment and expect long-term health benefits," Fox said.
Researchers from Duke University, Jackson State University, Wake Forest University, Boston University, University of Cincinnati, Howard University, Rush University, Xavier University, University of North Carolina, University of Minnesota and Morehouse College of Medicine are co-authors on the paper.
The Jackson Heart Study, a population-based longitudinal study conducted through a collaboration between UMMC, Jackson State University, Tougaloo College and the National Institutes of Health to discover and test best practices for eliminating disparities in cardiovascular health, is funded by the National Heart, Lung and Blood Institute and the National Institute on Minority Health and Health Disparities.


