Visual management boards give frontline staff care solutions forum

When the concerned mom of a newborn with a 103-degree fever called the Department of Family Medicine at the University of Mississippi Medical Center, the clinic quickly scheduled an appointment – but the standard workup calls for more urgency.

“For a child that age, it’s a more extensive workup in the Emergency Department,” said Dr. Shannon Pittman, the Alma Lowry Hill Chair of the Department of Family Medicine. “The suggestion from the provider is that we modify our triage tree to say that calls for patients of this age, with this fever, need to go straight to the nurse instead of scheduling an appointment.”
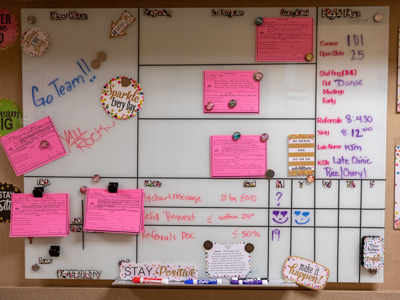
That’s just one example of a day-to-day change at the Lakeland and Flowood Family Medicine Clinics inspired by what’s called a visual management board, a large marker board mounted on a clinic wall next to patient rooms. It’s where clinic staff write down good ideas aimed at enhancing patient care by making it safer, more efficient and more effective.
Monday through Friday, shortly after 8 a.m., Family Medicine staff huddle around the board and track their progress on each idea or suggestion.
“The main goal is focused on improving efficiency and eliminating waste as we work to take care of our patients, and to empower the staff to take a critical look at their day-to-day activities and say, ‘How can I serve my patients better?’” Pittman said. “It’s an opportunity for the entire group to say they think an idea is worth their time and energy, and discuss how many people it will impact, how difficult it will be to make the change, and how quickly it can be done.”
Although the boards are used on some inpatient hospital floors, Family Medicine was the first clinic to use them. They’re in full view of Family Medicine patients in the spirit of transparency and patient interaction.
“We set the goal to roll this out to all adult ambulatory areas,” said Margaret Head, chief ambulatory officer for the adult hospitals. “Family Medicine was ahead of the curve and has been able to serve as a model for how to use it effectively.”

The boards are usually three feet by four feet, or four feet by six, depending on wall space, said Jeff Dunaway, director of performance improvement in the office of Chief Medical Officer Dr. Michael Henderson. Dunaway and his staff teach departments how to use the boards in addition to training others on the department level to do the same.

“Visual management boards are a well-established, tried and true tool in the ‘Lean Management’ toolbox that we have introduced to UMMC as a component of our high reliability/performance improvement journey,” Henderson said.
A board “facilitates communication and gives a voice to the front-line staff. It teaches them a standard way to solve problems, and it gives them a way and a place to look at their metrics,” Dunaway said.
The Family Medicine board is modeled on three “swim lanes” for three projects in the works. More ideas “are held in a ‘parking lot’ until a lane opens,” Pittman said. “The beauty of the board is that it allows you to see how the process moves forward. You always have a visual of the progress.”
Registered nurse Kim Clark has helped shepherd use of the Family Medicine board at the Lakeland clinic. She said she mentally rolled her eyes when she learned they’d be using the board in the midst of a busy clinic. She wondered if there was even time for employees’ voices to be heard.
The answer, she found, was yes.
Clark wrote a detailed memo explaining the new visual culture. “The time spent daily navigating the board is less than 15 minutes, and most days, it runs for less than eight minutes,” she observed. “In an arena where communication can be a difficult challenge, we are filling the gaps.”
One of the first ideas making it through the swim lanes was creation of a color-coded file system, hung on patient exam room walls in a pocket formation, to hold the most common forms and educational materials distributed as part of a visit. “Nurses found that they were constantly going back and forth to their bays to get forms,” Pittman said. “Now, the forms are in the room.”
The easy access “has directly resulted in reduced time wasted for both nurses and providers,” Clark said. “Indirectly, this addition has increased our patient education and satisfaction.”
Thanks to the work of Family Medicine, a number of other departments are rolling out, or preparing to roll out, visual management boards in their clinics. “We have already been sharing our lessons learned and tools with others,” Pittman said. “We’ve had multiple visitors to our board and our rounds. The goal from Margaret’s perspective is to share this as a tool to really engage staff moving forward.”

Among the earlier visual management board users is the second floor of Batson Children’s Hospital, which has held a daily 8:45 a.m. safety huddle at its board since October 2018. Staff there have made 27 changes based on ideas they submitted, said nurse manager Wesley Smith.
Many of the ideas were dubbed “just do its” because they take little time and effort, but offer good benefits to patients and caregivers, Smith said. For example, staff placed a coffee maker in a family waiting room to be fired up by a technician early in the morning, which is busy for caregivers, but also the time when family most often want coffee.
Another “just do it” that directly benefits patients: Staff installed hooks on the wall outside each patient room so that physicians can hang their white coats on them before entering. “The sleeves of white coats can be dirty,” Smith said. “This is a good move for isolation patients and for infection prevention.
“This gives the staff the chance to see the process, and they can take ownership,” Smith said. “If I want to buy something for the unit, the staff might think that’s easy, but in reality (the process) might not be.”
That can also be true in the ambulatory setting, Pittman said. “Employees might say, ‘This seems straightforward to me, but why does it take management so long to get it done?’ This can be a tool to manage workplace concerns and to move people from complaining to a solution-oriented environment.”
The first visual management board was used in summer 2017 in Batson’s perioperative unit, Dunaway said, and “it’s grown from that.
“We want all departments to understand it and find value in it,” he said. “It’s a tool for them to latch onto for the purpose of training, conversations around high reliability, and metrics to drive improvement. This is truly a bottom-up approach: We offer this to you, and if you find value in it and want us to train you, we will do that.”
Pittman said she’s heartened to see her Lakeland staff using the boards as an opportunity to build community.
Clark came up with a huddle break tradition of team members “putting all their hands together and saying, ‘Ubuntu!’” Pittman said. “That’s a Zulu word that means ‘humanity.’ It’s also translated as, ‘I am because we are.’
“This helps us to really come together and talk about how to serve patients, with the affirmation that we are a family and a community.”

