Immunotherapy research led by UMMC cancer center director offers patients new hope
Medical Center faculty and staff often are recognized regionally, nationally and internationally for their academic or medical achievements. These accolades place UMMC among health science centers worldwide.
Immunotherapy research led by UMMC cancer center director offers patients new hope
Women with certain types of advanced ovarian cancer may have a new personalized treatment option available to them following a clinical trial led by the director of the UMMC Cancer Center and Research Institute.
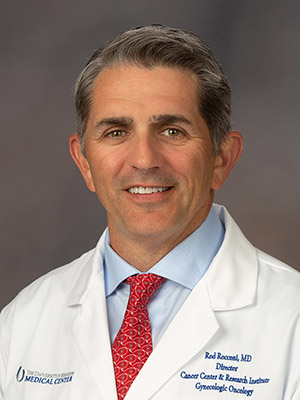
Dr. Rodney Rocconi, Ergon Chair of Cancer Research, was the lead investigator in a clinical trial that helped earn the U.S. Food and Drug Administration’s Regenerative Medicine Advanced Therapy (RMAT) designation for Vigil—a groundbreaking personalized immunotherapy for advanced ovarian cancer.
RMAT status, created under the 21st Century Cures Act, is reserved for regenerative therapies that show strong potential against serious or life-threatening diseases. It comes with an expedited path through FDA review, more frequent agency guidance and the possibility of accelerated approval.
Vigil, developed by Gradalis, Inc., is made from each patient’s own tumor cells. In the lab, scientists pinpoint the tumor’s clonal mutations—the core genetic changes driving the cancer—then engineer the cells in three ways: to target those mutations with precision, to boost immune activity so the body mounts a strong, localized attack, and to block TGF-beta, a protein that helps tumors hide from the immune system.
Rocconi compares it to tuning up a race car. “We plug in the GPS so it knows exactly where to go, we put the pedal to the metal to rev up the immune system, and we cut the brake lines so the cancer can’t slow it down.”
The trial tested Vigil as a maintenance therapy for women with advanced ovarian cancer after surgery and chemotherapy. Every participant received standard treatment first, then was randomly assigned to Vigil or a placebo injection.
Researchers discovered that the most significant results occurred in patients with high levels of clonal mutations and homologous recombination proficient (HRP) tumors—a particularly treatment-resistant subgroup. Vigil extended survival by more than four years compared to placebo patients.
“This is the first time in nearly 20 years we’ve seen a meaningful change in outcomes for HRP ovarian cancer,” Rocconi said. “It’s a huge step forward for a group of patients with an urgent, unmet need.”
Vigil also proved to be extraordinarily safe. Across thousands of injections, there were no severe side effects. The most common reaction was mild irritation at the injection site, which occurred just as often in the placebo group. Treatment is a simple monthly shot given for four to twelve cycles.
Rocconi emphasized that the trial’s success goes beyond ovarian cancer. “This shows that a truly targeted, patient-specific immunotherapy can work, even in cancers that don’t usually respond to immune therapy,” he said. “It opens the door to using this approach in other tumor types.”
With RMAT designation secured, Vigil is now on a faster track toward potential FDA approval, bringing new hope to women—especially those with the most treatment-resistant forms of the disease.


