Monitoring diabetes patients remotely key to better disease management
But it hasn’t always been that way. “I really didn’t take care of it, and my sugar was running high,” said Rhodes, a retiree who lives in Ripley in rural Tippah County. “I finally made my mind up that I was going to take it seriously and to discipline myself.”
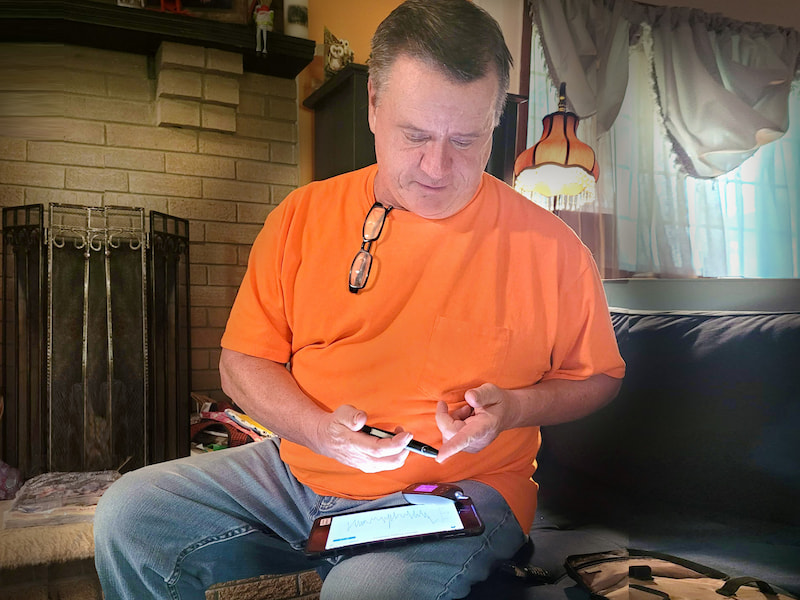
Rhodes is making good progress on managing his disease and maintaining a healthy lifestyle with help from remote patient monitoring offered through a partnership between the University of Mississippi Medical Center and North Mississippi Primary Health Care, a Federally Qualified Health Center that serves multiple cities in that region.
The goal: Eventually help at least 1,000 patients who cope with diabetes to monitor and control their disease, via providers at UMMC’s Center for Telehealth, so that they don’t end up in an emergency department or require a hospital stay.

Using cellular-enabled tablets the Center provides as long as the patient is enrolled in the program, Rhodes and other patients in the program record their glucose level. The information is transmitted directly into their UMMC electronic record so that Center providers can medically manage them between visits with their local providers.

The Center approached NMPHC as part of efforts to increase collaboration with Mississippi’s federally qualified health centers, said Gregrey Hall, the Center’s director of telehealth IT.
It’s a win-win for patients and NMPHC. “We are getting data from the patient’s home on a daily basis,” he said. “Our nurses are looking for trends in their blood sugar levels. If it’s slowly going up, they will call that patient. The patient knows that someone is looking out for them and cares what their health looks like on a daily basis.”
Hall also tracks financial data, evaluating the program to see if it’s saving money. “That’s the other side of this – the financial impact on the health system,” he said.
“We know this works,” Wright said. “We’re trying to get more and more data so that we can show people the benefits of this type intervention.”

Mississippi ranks first in the nation for overall diabetes prevalence, with more than 13.6 percent of the population affected, most recent data from the Mississippi State Department of Health shows.

And of that number, Nunnally said, “either they don’t have a (blood sugar) test on file with us, or the A1C test that measures their average sugar shows that it’s way too high.
“This program makes sense because the distance and access barriers can be overcome,” he said. “Sometimes, it’s hard to teach a patient outside of a clinic what can help them. This gives them access to education so that they can better manage their disease.”
“This gives us another set of eyes so that we can look at what our patients are doing every day, and that makes a big difference when it comes to their sugar,” Nunnally said. “If they are continuously having high sugar and we only see them every three months, we’ve lost ground.”
“By me taking this on, I’ve dropped (my blood sugar level) from 330, to 200, to down in the 100s” Rhodes said. “I’m proud of myself.” The Center’s blood glucose level goal for patients is less than 140, Tucker said.
“It’s hard to ask a patient to come to the doctor,” Nunnally said. “There are so many barriers, including transportation. Having them connected by technology so that UMMC providers can intervene – that’s going to make a difference in our patients being able to have their sugar under control, and to have better outcomes.”
Eventually serving 1,000 patients is a realistic goal, Nunnally said. “We probably have that number of patients whose sugar is not well controlled, or that is not monitored regularly,” she said.
In his retirement, Rhodes is tending to a garden that produces a healthy and nutritious assortment of green beans, wax beans, snow peas, radishes, romaine lettuce, squash and tomatoes.
He said he appreciates “that invisible person” who keeps him on track in his quest to control his diabetes.
“Them being there every day for me has been a big plus,” Rhodes said. “When you start seeing positive numbers, that’s encouraging.”


