Typically disregarded brain lesions may warn of heightened stroke risk
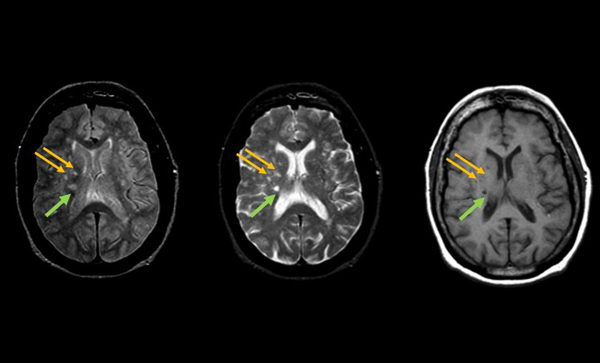
Scientists from the University of Mississippi Medical Center (UMMC) and colleagues found that very small brain lesions noted on brain imaging that would typically be disregarded by clinicians are associated with a heightened risk of stroke and death. The findings are in the July 7, 2015 issue of Annals of Internal Medicine.
The discovery about these tiny lesions — areas of the brain where tissue has been damaged by injury or disease —may help physicians identify people at risk of stroke and death as early as middle age, even when they are displaying no symptoms of cardiovascular disease.
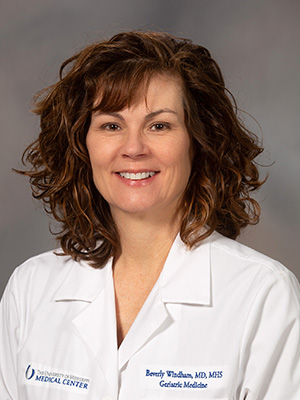
"The lesions on the brain imaging were very small, less than 3 millimeters, and are typically ignored in clinical practice," said lead study author Dr. Gwen Windham, an associate professor of internal medicine and geriatrics at UMMC. "This is because we have been uncertain as to their meaning; no studies have looked to see if these very small lesions are related to important clinical outcomes. Our findings suggest they are at least as important as 3 millimeter or larger lesions that are typically considered abnormal, even in absence of other lesions."
The researchers analyzed brain magnetic resonance imaging (MRI) data from nearly 1,900 individuals participating in the Atherosclerosis Risk in Communities (ARIC) Study who were 50 to 73 years of age with no prior history of stroke, tracking their health over about 15 years.
Risk of stroke or stroke mortality in people with small lesions was three times greater compared with people with no lesions. People with both very small and larger lesions had seven to eight times higher risk of these poor outcomes.
"Some of these lesions are so small they have the resolution of a single pixel," said Dr. Thomas Mosley, director of the Memory Impairment and Neurodegenerative Dementia (MIND) Center at UMMC and senior scientist on the study. "In clinical practice, we would typically ignore these tiny lesions as insignificant. The assumption has been that these very small lesions probably are not particularly consequential, but, in fact, they appear to be."
Although clinicians and researchers tend to dismiss very small cerebral lesions, the current findings suggest the practice could warrant reconsideration, the researchers said.
More than 800,000 strokes occur each year in the United States, according to the National Institute of Neurological Disorders and Strokes. Strokes are a leading cause of death in the country and cause more serious long-term disabilities than any other disease.
Knowing that these tiny areas of damaged tissue indicate increased risk of stroke in apparently healthy people could be important to help people maintain physical function and cognitive ability as they get older, said Windham, who also serves as director of the MIND Center clinic.
"We know that modifiable risk factors like hypertension and diabetes are associated with the larger structural changes in the brain, and those larger lesions are not only associated with stroke risk but with mobility impairments and cognitive impairments as well," Windham said. "Ongoing trials may determine whether treatment of risk factors, like high blood pressure, reduce the incidence of these lesions, stroke and associated death and disability."
The discovery about stroke risk grew from work at the MIND Center, a cutting-edge Alzheimer's disease research institution at the University of Mississippi Medical Center.
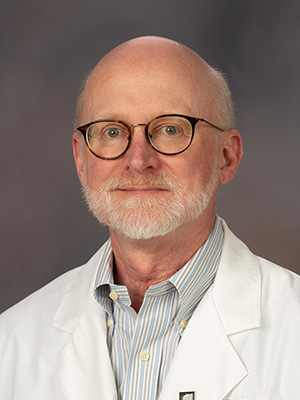
"We are trying to identify the factors that hasten cognitive decline and the onset of Alzheimer's disease, and it may be one of our best prevention strategies is aggressive control of cardiovascular risk factors early in life, meaning in middle age," Mosley said. "In Mississippi, the mortality rate from heart disease and stroke is among the highest in the nation, so we've been interested in this connection between cardiovascular disease, brain aging, and Alzheimer's disease for a long time."
Prior studies have typically focused on older, largely white patient samples, but this study was aimed at understanding brain changes from an earlier age and recruited a more middle-aged, bi-racial sample.
Half of the sample participants were black, who generally have higher rates of stroke and cardiovascular disease for reasons that remain unclear. Identifying early markers of at-risk individuals could significantly impact the public health burden of cerebrovascular disease in all ethnic groups, the researchers said.
"People don't routinely have MRIs, but when they are necessary, taking note of these small lesions could provide valuable information about future risk," Windham said. "It's similar to knowing about a patient's history of high blood pressure or family history of heart disease — it may influence treatment decisions."
In addition to researchers from UMMC, the study was co-authored by scientists from Johns Hopkins University, the University of Washington Medical Center, Mayo Clinic, and the University of North Carolina at Chapel Hill.
The study was funded by the National Heart Lung and Blood Institute of the National Institutes of Health.


