OB-GYN integrates nurse-midwifery into maternal health care
As maternal mortality continues to rise across the country, barriers to comprehensive maternal care are particularly evident in Mississippi. With the highest infant mortality rate, preterm birth rate and low-weight births in the nation, the state is in dire need of solutions.
In response, the University of Mississippi Medical Center is on a mission to increase and support the growth of nurse-midwifery throughout the state, beginning with the addition of two nurse-midwives to the UMMC Department of Obstetrics and Gynecology.
The department is drawing upon its historical legacy of leadership in the field of nurse-midwifery to offer a beacon of hope for the future. Dr. J. Martin Tucker, professor and chair of obstetrics and gynecology, recruited Janice Scaggs, certified nurse-midwife, to help integrate midwifery back into the system.
Scaggs hopes to see the program grow and help change the public perception about midwifery.

“Part of my job is to educate people on what a midwife is and specifically what my job as a nurse-midwife is because there are a lot of misconceptions,” she said. “I think many people don’t understand that nurse-midwives have graduate-level education—and that’s at the entry level. A lot of us actually have doctorate degrees. Another misconception is that we only practice home birth and don’t support women in hospitals. Over 90% of nurse-midwifery attended births in the U.S. are in hospitals, 8% in free-standing birth centers and less than 1% in homes.”
Scaggs said currently there are no free-standing birth centers in Mississippi or nurse-midwives who provide care in the home.
“We support the woman’s choice of having nonpharmacologic support, IV pain medications or epidurals during labor and birth. Many people also don’t know that we provide primary care and gynecologic care,” she said.
In 2001, Scaggs began her clinical practice as a certified nurse-midwife in Greenville, North Carolina. However, when she returned to Mississippi 15 years later, she faced challenges in finding work in the field. To gain a better understanding of the current situation and develop nurse-midwifery in the state, she pursued her doctorate—graduating in May 2020 from University of Southern Mississippi.
“I returned to bedside nursing in a newborn nursery and was present for births, watching physicians performing the tasks I had always handled,” Scaggs said. “This experience brought me humility. Obtaining my doctorate and working in a community hospital allowed me to connect more closely with nurses, physicians, administrators and educators. I know now that was a crucial step in planning to reintroduce a profession that had been missing at UMMC for decades."
When she joined UMMC in fall 2020, Scaggs said she spent the first six months observing daily operations within the OB-GYN department. “I was following nurses; lactation consultants; physicians, observing the women’s urgent care and post-partum units, and trying to figure out where midwifery could fit within the system,” she said.
As she became more familiar with the structure and began integrating practice with residents, nurses and students, Scaggs and Tucker decided to develop a nurse-midwifery clinical advisory committee to formalize a long-term strategy for the department. The multidisciplinary committee spent about a year addressing solutions to anticipated barriers. Then, working with an accomplished nurse-midwifery consultant company, the committee developed a plan.
Over the course of five years, the plan is to introduce a minimum of eight certified nurse-midwives into UMMC hospitals and clinics in the metro area and surrounding counties, with the aim of offering round-the-clock service by 2027. As part of the department's growth, the nurse-midwives will support nurse-midwifery students, medical students and resident clinical education.
Tucker said it has been a pleasure working with Scaggs and is grateful to her for turning his dream into a reality. “[We] have a unique opportunity to integrate midwifery services into our clinical care model,” said Tucker. “Having certified nurse-midwives as team members and collaborators enhances patient care as well as student and resident education.”
According to the World Health Organization, midwifery is an evidence-based approach to reducing maternal and neonatal morbidity and mortality. It suggests that midwife-led care contributes to more efficient use of health system resources by decreasing unnecessary interventions like cesarean sections for low-risk deliveries, epidural use and instrument-assisted births.
Today, there are only 20 to 30 certified nurse midwives licensed by the Mississippi Board of Nursing and even fewer practicing in the state, with many students opting to seek employment in other states upon graduation. Currently only about 2% of births in Mississippi are attended by midwives, but evidence suggests that midwife-led care for women yields positive birth outcomes.
As of 2021, just 12% of births in the United States were overseen by midwives – most of these by certified nurse-midwives and fewer by certified midwives, certified professional midwives or direct entry midwives. Although midwife-assisted births constitute a minority of births in the country, there is compelling evidence that the integration of midwifery into a health care system enhances maternal and neonatal outcomes.
Studies show that the use of midwives during pregnancy significantly reduces low birth weight and preterm birth rates, increases breastfeeding rates and improves psychosocial well-being outcomes such as postpartum depression. Experts predict that if midwifery care in the U.S. increases from 8.9% to 20% by 2027, it could result in $4 billion cost savings, 30,000 fewer preterm births, and 120,000 fewer episiotomies.
Midwifery, an ancient profession with a history spanning millennia, traces its roots back as far as 40,000 B.C., having been embraced across diverse cultures worldwide. Midwives, held in high esteem in most societies, extended comprehensive physical, mental, emotional and spiritual care to mothers from conception well into the postpartum period. Historically, childbirth was a ceremonious affair, predominantly overseen by women who passed down their wisdom as primary caregivers in their communities.
However, a significant shift occurred in the 18th century when physicians began taking a more substantial interest in the field of childbirth.
This formalization of nurse-midwifery in 1925, while contributing to the health care landscape, left limited space for the practice traditionally dominated by Black women, leaving lasting impacts on the African American population in the United States. However, that change was more slowly realized in the southern states, where as late as the 1930s, 75% of births were still attended by Black midwives.
By 1947, Mississippi stood out with 58% of births taking place at home, compared to just 10% nationwide, and predominantly under the care of midwives. However, as hospital births became more prevalent and educational barriers persisted, the practice of apprentice-trained community midwives saw a steep decline.
In 1969, in the midst of an unprecedented maternal health crisis, a nurse-midwifery education program was established at UMMC with support from the County Health Improvement Program. The modules developed by Mississippi nurse-midwives laid the foundation for education and practice standards for all nurse-midwives in the U.S., including a master’s level education for entry into practice.
Subsequently, programs at institutions like Emory and the University of Pennsylvania, among others, followed suit, building on the blueprint provided by UMMC nurse-midwives. Although the program laid the foundation for standardization of nurse-midwifery education across the country, it closed in 1979 due to a lack of funding, legislative barriers and lack of advocacy from physicians at the time.
If the initial efforts of reintroducing midwifery prove successful, UMMC will explore further expansion of services and educational opportunities in Mississippi, specifically in areas that are considered maternity deserts. With this roll-out in motion, the department has recently welcomed a second certified nurse-midwife, Kim Rickard, to the team.
Currently patients can be seen by a nurse-midwife at the UMMC Grant’s Ferry location or in Wiser Women’s Hospital where they provide patient care three days a week.
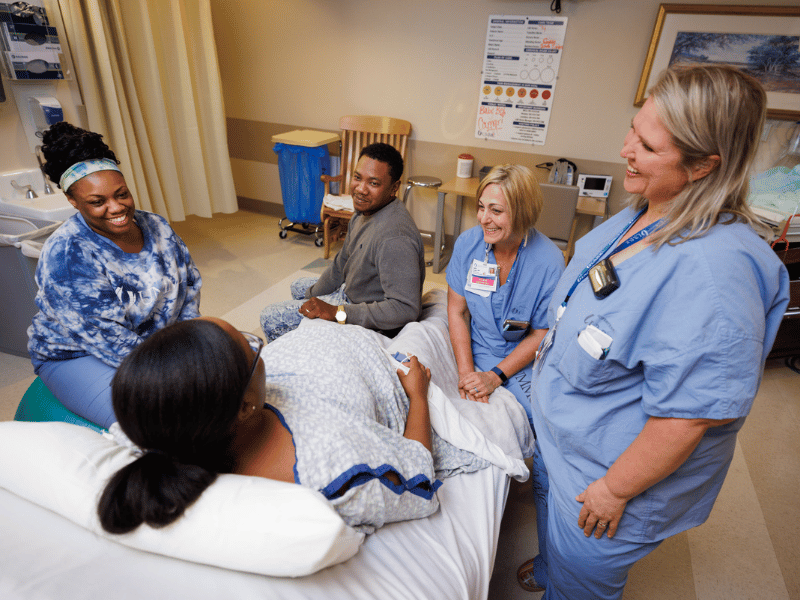
The nurse-midwives' significant influence on the department is evident as they strive to empower patients as an active partner in their care, allowing them to make decisions based on recommendations of the best evidence. The addition of Scaggs and Rickard has proven to be an asset as they also function as a bridge between providers, nurses and the rest of the delivery team.
Nital Patel, labor and delivery nurse manager, said that as the first midwife she has worked with, Scaggs proves that the integration of midwifery supports the entire department.

“At first, I wasn’t sure how it was going to look because we take care of a lot of high-risk patients,” she said. “But since Janice joined us, and now Kim, I see the value that they bring. Janice has offered a different perspective to both the nurses and providers because she has been both. She has enhanced communication across the department because she acts as a translator for everyone.”
Scaggs was recently recognized by The American College of Obstetricians and Gynecologists-- receiving the 2023 National Faculty Award for Excellence in Resident Education, voted on by the UMMC ob/gyn residents.
Scaggs and Rickard said they have felt very supported by the department and hospital administration since arriving.
“We share the goal of improving maternal morbidity and mortality and have established a strong partnership and team-based approach to achieve these goals,” Rickard said. “As a native Mississippian, I am excited to move back home and to be here helping to grow nurse-midwifery in our state. I moved from an out-of-state practice that was able to provide 24/7 nurse-midwifery care and am looking forward to the growth of UMMC midwifery service where we will eventually be able to provide that for women in Mississippi.”


