Sepsis study’s design “future” of clinical trials
A phase-II, multi-center trial for a septic shock treatment led by the University of Mississippi Medical Center is a model for a new way to conduct clinical trials with critically ill patients.
Published in JAMA Network Open December 21, the RACE trial, short for Rapid Administration of l-Carnitine in sEpsis, is one of the first adaptive clinical trials funded by the National Institutes of Health.
The leading cause of death and most costly condition in intensive care units, sepsis, which is when the body has a systemic overreaction to an infection, has a mortality rate around fifty percent. In severe cases, the low blood flow throughout the body can lead to organ failure.
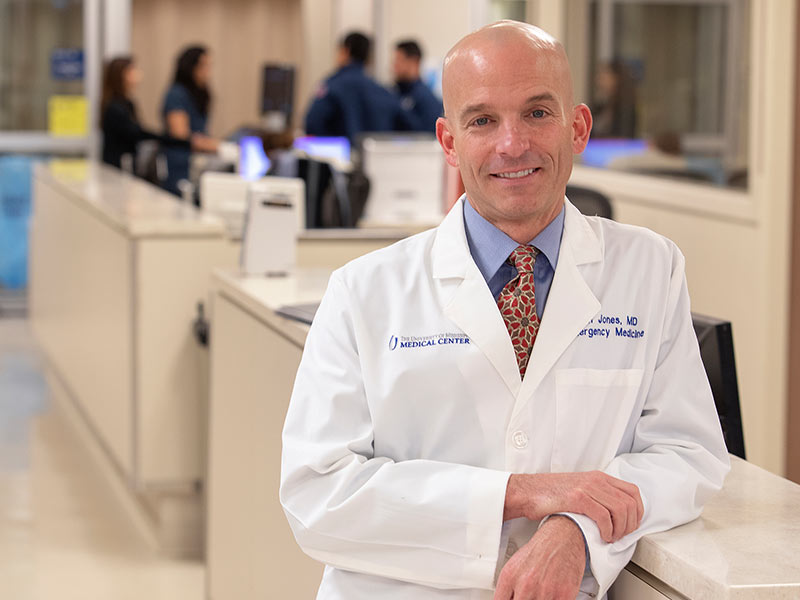
“One of the primary metabolic issues in sepsis is that the body switches to its fuel source entirely to carbohydrates,” said Dr. Alan Jones, professor and chair of emergency medicine at UMMC, was the principal investigator for the trial. This leaves fatty acids circulating in the body, potentially building to toxic levels.
RACE tested carnitine, a compound in the body that helps shuttle fats into mitochondria for fuel. A smaller study associated this treatment with the potential to decrease organ failure and death from sepsis.
“There is evidence that carnitine is depleted in sepsis, so administering carnitine may mitigate some of the metabolic effects,” said Jones, who has led multiple sepsis-related studies.
Jones and his team drew blood from the participants to measure sequential organ failure assessment, or SOFA, 48 hours after administering carnitine through IV infusion. They also tracked 28-day mortality.
While the trial did not show significant improvements with carnitine treatment, its design sets it apart. The Food and Drug Administration has touted adaptive clinical trials as a way to decrease costs and accelerate the timeline for drug and device development.
“If we can allocate patients into the arm of the trial that is working best, we can more efficiently utilize patients and resources, and perhaps benefit more patients,” Jones said. This is particularly valuable when trying to treat a condition as life-threatening as sepsis.
“The adaptive trial model has been used in some clinical scenarios, but our study is among the first to apply it in a critical care setting,” Jones said.
Adaptive designs allow researchers to plan their studies with a level of flexibility. They can change doses, study size, or another factor based on preliminary findings. Typically, changing the rules of the game mid-experiment is bad practice in science. It can compromise results. However, sufficient planning and statistical know-how can allow for built-in alterations.
Jones’ study design allowed the number of individuals in each treatment group to be adjusted in proportion to the likelihood a treatment would improve SOFA. The 250 RACE participants were assigned one of four doses of carnitine: 18, 12, six, or zero grams. A traditional trial design would have put about the same number of participants in each arm. In the adaptive design, this happened with the first 40 patents only.
Then, statisticians checked the data to see which treatment had the highest probability of improving SOFA. The high dose showed the most promise, so a greater proportion of the next 12 participants received that treatment. The study repeated this process of assessing and allotting until it was finished, with 106 participants receiving the high dose, 34 the medium, 35 the low, and 75 the placebo in order to maintain a control group.
The study maintained its blinding, meaning neither investigators nor participants knew who received which treatment. Only the statisticians saw the early data and only the pharmacists knew the contents of the IV bags.
The team found that the high dose had a 78 percent probability of being better than the placebo at improving SOFA, which was lower than the 90 percent threshold they decided would be needed to justify proceeding to a larger, phase-III trial of carnitine.
Jones notes that while the trial results were not statistically significant, there was a five percent mortality decrease among patients who received the high l-carnitine dose and completed the entire trial per protocol. In a clinical setting, that five percent can be meaningful, Jones said.
Dr. Richard Summers, associate vice chancellor for research, said Jones’ study is an example for how to do adaptive clinical trials trials properly.
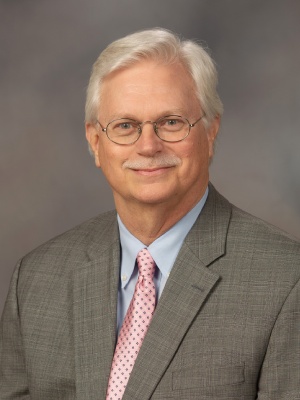
“I was recently contacted by a clinical researcher at Johns Hopkins who told me he was seeking approval from the FDA for an investigational new drug and they advised him that his clinical trial protocol needed to follow the ‘Jones’ method,” Summers said.
“Being a unique NIH-sponsored adaptive clinical trial makes the RACE trial another UMMC first and pioneers the way FDA clinical trials will be performed in the future,” Summers said.

Sepsis trials are “notoriously negative,” said Dr. Jeffrey Kline, vice chair of research in the Department of Emergency Medicine at Indiana University and a co-author of the study. “The trend toward improvement was surprising to me. Sepsis is so multi-factorial, to think that one molecule can fix it or create any benefit is surprising. The hypothesis was highly justified.”
Jones and collaborators want to look at participants’ metabolic profiles to determine if there are difference between those who improve with carnitine supplementation and those who do not.

“Figuring out who is going to benefit from a specific treatment and getting the right treatment to the right patient is the future of sepsis research,” said study co-author Dr. Michael Puskarich, an emergency medicine physician at Hennepin County Medical Center in Minneapolis and former UMMC faculty member.
In science, it’s important to publish non-significant findings. It promotes transparency and can steer researchers towards treatments that may be effective.
“In the scientific realm, most scientists are less invested in the outcomes and more in the question itself,” Jones said. “As we gather more data, we can hone in on the population where this treatment may be most useful. It’s another piece of the puzzle.”
Additional study authors represent Beth Israel Deaconess Medical Center; University of Florida College of Medicine-Jacksonville; Carolinas Medical Center; University of California-Davis; Wayne State University; Christiana Care Health Services; University of Alabama School of Medicine; University of Texas Health Science Center-Houston; Northwestern University; Cooper University Hospital; and Berry Consultants.
The National Institute for General Medical Sciences funded the study.


