From COVID-19 variant to variant, critical care providers fight to save lives

Six months pregnant with her first child, hospitalized and her lungs ravaged by COVID-19 and a cough that wouldn’t quit, Amber Rodgers made a terrifying decision.
“The doctor came in and was talking about the ventilator,” Rodgers, 21, said of her critical care physician at the University of Mississippi Medical Center. “He really didn’t want to wait until I got worse.

“I asked if there were any other options for me to get better. He said, ‘That’s the last option.’”
There wasn’t much time to take it all in. “I was even more scared because I didn’t want to be on the vent. I didn’t know how long I’d be on it, or how it worked. And, the baby,” said Rodgers, then unvaccinated and admitted to the hospital Dec. 8, 2021.

But, she agreed. During last summer’s Delta surge, the vast majority of pregnant moms with COVID-19 who were mechanically ventilated at the Medical Center didn’t survive. “That percentage has dropped. Omicron has not been affecting our mothers like Delta did, at this point,” said Dr. Rachael Morris, associate professor of obstetrics and gynecology and Rodgers’ maternal-fetal specialist.
Rodgers is in the small percentage of expectant mothers who got to go home after mechanical ventilation. “We are thankful for those very small moments,” Morris said of the survival of Rodgers, who had no other medical problems except mild obesity.
Regardless of the variant of COVID-19, hundreds of patients have transitioned from battling mild symptoms to requiring hospitalization and critical care. This is when the Medical Center’s critical care team and other specialists exhaust every option to save lives.
Since the pandemic began, more than 1,000 adults with COVID-19, most of them also coping with chronic illnesses and comorbidities such as diabetes, heart failure or morbid obesity, have received ICU care at the Medical Center. That’s in addition to more than 100 pediatric COVID-19 patients, some who also had pre-existing illness or comorbidities.

A few hundred of the adult COVID-19 patients spent time on a ventilator, estimates Dr. Andrew Wilhelm, associate professor and chief of the Division of Pulmonary and Critical Care Medicine. On Jan. 24, he was sharing in the care of 26 adults confirmed with COVID-19 in the ICU. Another 43 adults were coping with COVID in a regular hospital room.
Nearly a month ago, on Dec. 27, there were nine in the ICU and 19 on patient floors.
For the Medical Center’s adult patients with COVID-19 so desperately ill that mechanical ventilation is their best chance, the majority are unvaccinated – but not always. During the ongoing Omicron variant surge, “we have seen a mix of unvaccinated and fully vaccinated patients in the ICU on mechanical ventilation,” said Dr. Bhagyashri Navalkele, an assistant professor in the Division of Infectious Diseases and medical director of infection prevention and control. “Almost all of the vaccinated and fully vaccinated patients had associated comorbidities.”
There have been rare cases of intubated COVID-19 patients who were boosted in addition to being vaccinated, “but it’s extremely rare to see one without comorbidities,” Navalkele said.

The Omicron variant is much more contagious but tends to result in lower ICU numbers and shorter hospital stays. But if you’re sick enough for ICU care, “it’s just as bad as Delta,” Dr. Louann Woodward, UMMC vice chancellor for health affairs and dean of the School of Medicine, said at a Jan. 11 news conference.
Mortality rates at UMMC for intubated COVID-19 patients have varied since the beginning of the pandemic, but they match the national average of about 30 to 50 percent, with the higher rate applying to patients who must have both ventilation and kidney dialysis, Wilhelm said. And although the national average has fluctuated from variant to variant, fewer COVID-19 patients on a ventilator isn’t translating into fewer of them dying.
Critical care team members including Wilhelm and Dr. Jessie Harvey, an assistant professor in pulmonary and critical care medicine and director of the Medical Intensive Care Unit, pull out all the stops to save their lives.
“Unfortunately, once someone gets to that point in a critical illness, there’s nothing new that will change the odds,” Wilhelm said. “Between the hospitalists, the infectious diseases team, the respiratory therapists, the pulmonology ICU team, the pharmacists and obviously the bedside nurses who have done this for the last two years, we work together to do the best we can.
“If we had a magic medicine, the conversation might be a little different.”
‘Often, they don’t come off’
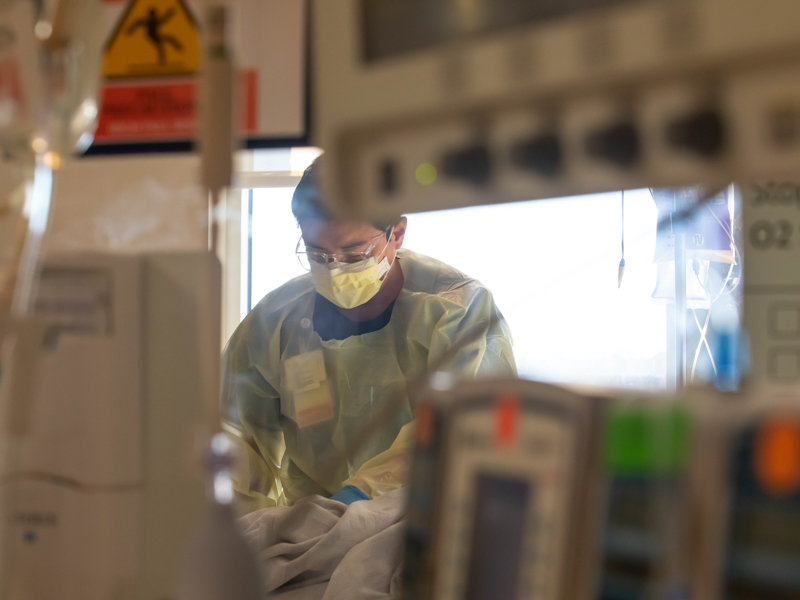
Walk down the hallway of any of the Medical Center’s intensive care units, and you will see patients through sliding glass doors who are intubated, or have a breathing tube inside their chest that rests right above their lungs.
Most don’t move. The fortunate ones will wake up.
“We will let COVID patients go a little longer before putting them on a vent. Once they go on the vent, a lot of the time they don’t do well, and often, they don’t come off,” Harvey said.
Not many people understand the process that occurs when mechanical ventilation is the caregiver’s last life-saving tool.
If a COVID-19 patient struggles to breathe, the first treatment is high-flow oxygen through a cannula under their nose to shoot up to 100 percent oxygen to their lungs. The next step up is BPAP, short for bilevel positive airway pressure. It forces air through a face mask into a patient’s lungs. It’s considered ventilation, but not as invasive as intubation.
“We try everything we can,” Harvey said. “We encourage them to sit up in bed, and to prone themselves (rotate lying face down and face up) to let different parts of their lungs ventilate.”
“If they’re on 100 percent oxygen and it’s not working, we have to make that decision: How can we best oxygenate our patient?” said John Brinson, a respiratory therapist and interim manager of respiratory therapy care.

If the patient’s breathing continues to deteriorate, the critical care team has one of its most difficult conversations. If the patient can communicate, they’re asked to give permission to be placed on a mechanical ventilator.
“We want to know their wishes. We talk to the family,” Harvey said. “We want to have the conversation before the patient gets too confused.
“My heart sinks a little bit. I’m always a little nervous, because these patients are so sick. It makes intubation more tricky,” she said. “We don’t want to put the tube in too early, but patients who refuse it and then decide later they want it are at much higher risk.”
“Getting to the point of a ventilator ... everyone on our team knows what that means,” Morris said.
“You’re probably not going to go home, no matter what we do.”

Most patients say yes to the vent. Some say no. And some say they don’t want it until their breathing gets to the point where they are gasping and they change their minds.
“We try to help them with options. We want to be honest, but we don’t want to take away hope,” Harvey said. “We need the hope, too.
“If they aren’t going to come off the vent, they won’t know it. I want this to be as peaceful and as calm as possible.”
If they’re able, patients are encouraged to call friends and family – “anybody they want,” Harvey said.
“You can see how scared they are that they won’t come off,” Harvey said. “If they’re not scared, they’re somber. By the time they get to this point, they don’t feel like they have that fight in them.”
When nothing else works
The process of mechanically ventilating a patient requires many hands, and for pregnant moms, the bedside team also includes both neonatal intensive care and labor and delivery providers. It’s not unusual for a mom or baby to become so unstable that an emergency delivery is required right there, in the moment.
The medical team builds up the patient’s oxygen as much as possible. “The process of putting them on the vent decreases their oxygen. We have to paralyze them to put the ventilation tube down their throat, and they won’t have any oxygen during that time,” Harvey said.
Through their IV, a patient receives a sedative and usually, a drug to paralyze them. “If a patient is fighting, you sedate first, then paralyze,” Brinson said.
A patient can stay on the ventilator for days to months, and how their oxygen is managed is tailored to how well or how poorly they’re doing.
Many sedated patients are laid prone. It’s people-intensive, requiring four or five providers, fully dressed in PPE, to turn them over – as quickly as they can, because their vent must be clamped off during the process.
“You can imagine when we have a lot of COVID patients how long it takes away that group from their other patients,” Harvey said.
The final treatment providers can try – generally for young people with few to no comorbidities – is extracorporeal membrane oxygenation, or ECMO. It’s a life support machine used in addition to a ventilator. In short, it takes the blood out of a person’s body, oxygenates it, then pumps the blood back into the body. UMMC is the only Mississippi facility with ECMO.
Watching and waiting
As days pass, a COVID-19 patient on a ventilator deteriorates. They may experience multi-organ failure. They could pick up bacterial or fungal infections or develop pneumonia or blood clots. Their limbs become too weak to function. They can experience brain fog and mental challenges. Some are on dialysis because their kidneys failed.
“Being on a vent is bad for your lungs. Being on ECMO is bad for your lungs,” said Brady Holder, a respiratory therapist and interim director of respiratory therapy.
“It’s a ticking time bomb,” Harvey said. “The longer you’re on the vent, the more worried we are that you won’t come off. Even if their lungs improve, it can take a very long time for them to regain the strength to come off a ventilator.”

If their oxygen saturation appears high enough, Brinson said, “we cut the sedation back and start to wake them up. We want them to start breathing over the ventilator. If they are sitting up in bed and ask you to pull out the tube, they’re probably ready.
“If we see they’re not ready, sedate them and let them rest until they are ready.”
When providers believe a patient won’t survive intubation, and when a patient or family “makes the decision not to press on,” Harvey said, the patient transitions to what’s called comfort care. It’s just that – keeping the patient comfortable until they die.
The IV is disconnected. Sedation, paralytics and antibiotics stop.
“We do not want them to struggle. We want them to pass naturally,” Harvey said.
But there are survivors.
Rodgers, who returned home Christmas Day, said there was no big reason why she hadn’t gotten the vaccine. “It hadn’t been out that long,” she said. And she’d had the virus before, very early in the pandemic.
Aurielle is due April 8. “I’m really lucky. I’m glad the baby didn’t have to be taken early and could continue to grow,” Rodgers said.
“When I got out of the hospital, I waited my 14 days, and I got the vaccine. I do not want to feel that way again, or end up in the hospital again.”


