Barriers to breastfeeding subject of three-year NICU study at UMMC

Improving the supply of mother’s milk for the unique needs of very low birth weight infants receiving neonatal intensive care and minimizing disparities that prevent mothers from providing milk is the subject of a quality improvement project at the University of Mississippi Medical Center.
Express Yourself Mississippi, a three-year quality improvement project funded by a $1,116,209 grant from the W.K. Kellogg Foundation, will identify disparities and conditions that can be obstacles to breastfeeding for the mothers of VLBW babies in all of the state’s 13 Level III and Level IV neonatal intensive care units.
The Express Yourself collaborative is geared toward provision of maternal milk and reducing related disparities for the very low birth weight (VLBW) infants at Level III and IV NICUs in Mississippi and in the greater New Orleans area, Massachusetts, Michigan, and New Mexico. The project is yet to begin in Michigan and New Mexico.
“Breast milk is the optimal form of nutrition for babies, especially in their first days of life,” said Dr. Mobolaji Famuyide, medical director of Children’s of Mississippi’s NICU, housed at Wiser Hospital for Women and Infants and principal investigator of the study. “For babies, breast milk is not only nutrition; it is medicine. Mothers transfer immune protective substances to their babies through breast milk to help their immune systems to develop.”
UMMC has the state’s only Level IV NICU, which provides the highest level of care. The state’s Level III NICUs, which provide care to babies born at less than 32 weeks gestation and babies born with critical illnesses at all gestational ages, include those in Gulfport, Tupelo, Meridian, Hattiesburg, Greenville and Jackson.
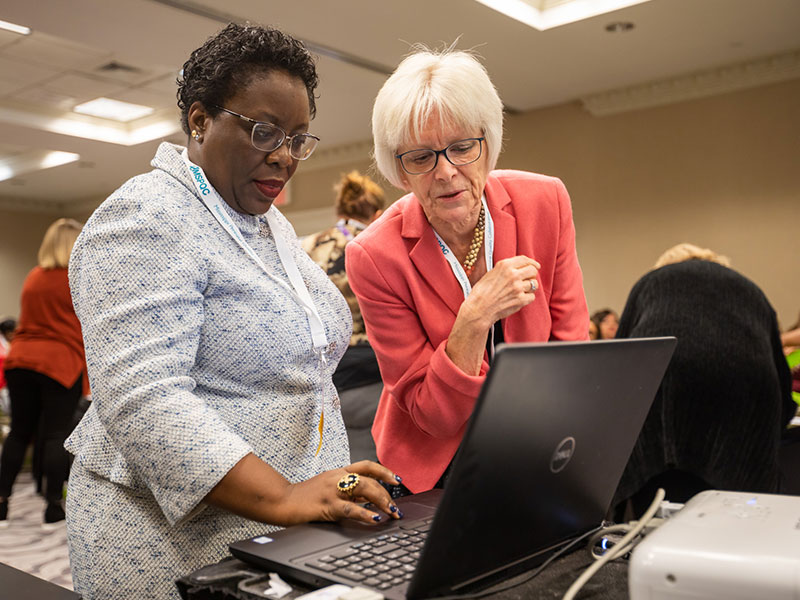
The project’s goal is to increase the number of mothers of VLBW neonatal intensive care patients who provide breast milk for their babies and identify disparities related to breast milk provision and ways they can be overcome. This will be done using quality improvement methodology and testing/implementing evidence-based interventions. Building a secure data infrastructure for future statewide quality improvement projects is a secondary goal of the project.
Nationwide, about 50 to 55 percent of mothers provide any breast milk for their very low birth weight infants at the point of discharge from the NICU. In Mississippi among NICUs participating in the Vermont Oxford Network, about 25 percent of VLBW babies were discharged home on any human milk in 2018, a number that Famuyide would like to see rise.
Disparities involving race, ethnicity, economic status and geography may play a role in whether a mother is able to provide breast milk. A mother having the ability to breastfeed after a baby comes home from the hospital can also be impacted by factors such as her own health, time, access to a breast pump, economic stress and working conditions, Famuyide said.
“Breastfeeding has been shown to be the best way to nurture babies, and babies in the NICU especially need the benefits of breast milk,” she said. In addition to giving these babies immune protective factors that help them fight infection, breast milk reduces the risk of necrotizing enterocolitis, a devastating disease that affects mostly the intestine of premature infants and can be fatal.
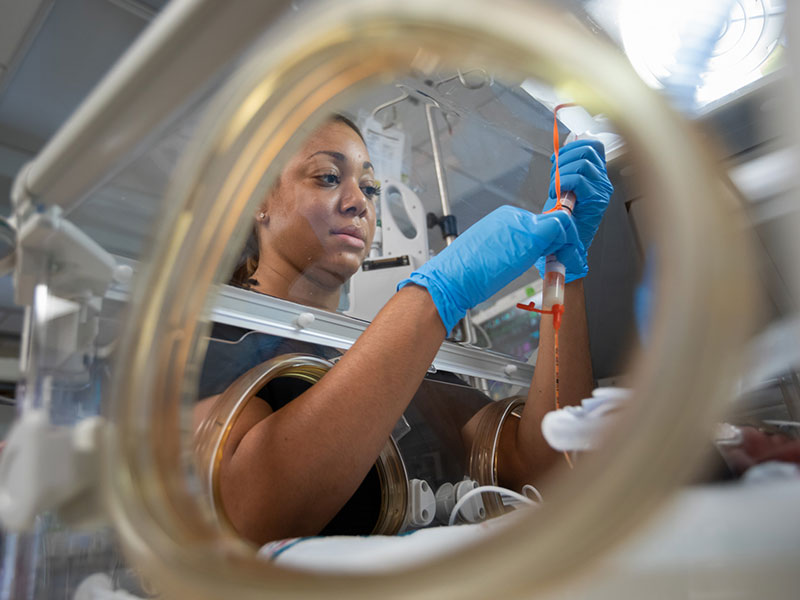
Many critically ill newborns are unable to breastfeed, so their mothers provide that nourishment through pumping. The milk can then be given to the newborn by bottle or through a feeding tube.
“It’s the best medicine a baby can get,” said Jamie Ford, a UMMC registered nurse certified in neonatal intensive care and International Board Certified Lactation Consultant who is the project nurse/coordinator for the Express Yourself Mississippi project. “When a mother has a baby in the NICU, providing breast milk is one of the only things she can do, and one of the most important things she can do, for her baby.”
Children’s of Mississippi has a room adjacent to the NICU where mothers can express milk for their babies, and mothers may also bring their babies frozen breast milk for later use.
“Ideally,” said Famuyide, “when pumping is successful, a mother would be able to not only provide enough milk for her own child but enough to also donate to the Mothers’ Milk Bank of Mississippi to help Mississippi babies.”

The nonprofit milk bank supplies NICU babies with breast milk when mother’s milk is not available. The organization screens donor mothers, then collects, pasteurizes and dispenses donor human milk to hospitals, following the guidelines of the Human Milk Banking Association of North America.
Neonatal intensive care is vital in Mississippi, where 14.2 percent of births are preterm, or at less than 37 weeks gestation, the highest rate in the country according to the 2019 March of Dimes Report Card.
Reaching mothers of babies receiving NICU care around the state will involve collaboration with the state’s hospitals as well as the Mississippi Department of Health and the Mississippi Perinatal Quality Collaborative, a statewide partnership that promotes best practices in maternal and neonatal health.
With the opening in fall 2020 of Children’s of Mississippi’s seven-story hospital expansion, 88 private neonatal intensive care rooms will allow mothers to stay with their critically ill newborns. The current NICU space was designed as an open bay for 30 babies, but today, about three times that number receive care there.
“This will be a dramatic change for our NICU families and staff,” said Famuyide, “and it will increase the likelihood that mothers will get the support they need to provide the nutrition their babies need.”
Mississippi has steep challenges in the health of mothers and their babies, she said, “but we think through Express Yourself and collaboration among our state’s NICUs and care providers, best practices can be identified and we can give our state’s babies the best possible start.”


