Study examines weight-loss surgery's potential effects on offspring
Published in News Stories on December 07, 2015
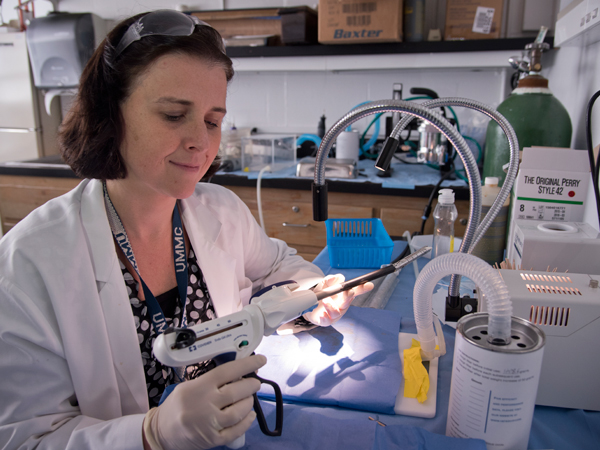
Women who have weight-loss surgery experience health benefits beyond lower weight, such as lower cholesterol and higher glucose tolerance. However, children born after their mother's surgery could face long-term health consequences including obesity and diabetes, says University of Mississippi Medical Center's Dr. Bernadette Grayson.
“The surgery treats obesity, but some of the post-surgery effects have not been vetted,” said Grayson, an assistant professor of neurobiology and anatomical sciences. She presented some of her recent findings as an invited talk at the American Physiological Society's conference titled Cardiovascular, Renal and Metabolic Disease: Physiology and Gender, held in Annapolis, MD on Nov. 19.
Grayson is a neuroscientist who studies metabolic syndrome, a group of diseases including obesity, diabetes and hypertension. In the lab, she uses female rats to study the effects of vertical sleeve gastrectomy (VSG) on reproductive biology. She looks at the long-term health of the offspring born post-surgery.
According to Grayson, changes to the maternal environment post-VSG - particularly in the placenta - may limit the pups' growth and lead to metabolic syndrome later in life.
“I don't know of any other groups who do this type of research,” Grayson said.
During VSG, a surgeon removes 75-85% of the stomach and reseals it, creating a tube-like sleeve instead of the stomach sac. This initially limits the amount of food a person can eat, so they consume fewer calories and lose weight. However, the reason for this long term weight loss is still not well known.
A typical patient loses more than half of their body weight over a three-year period. The procedure usually has few long-term complications.
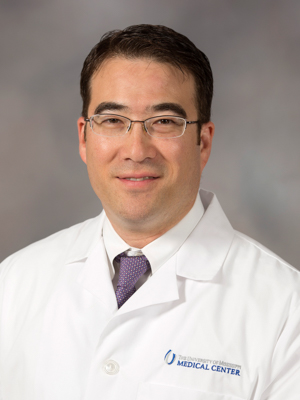
Vick
Dr. Kenneth Vick, professor of surgery at UMMC, says VSG makes up 85-90% of bariatric surgeries performed at the hospital.
Vick says some women may consider pregnancy 12-18 months after surgery. “Fertility may actually improve after surgery,” Vick said, since obesity is a risk factor for infertility.
Studies show that these women have lower rates of pregnancy-related complications like preeclampsia and gestational diabetes than obese women who haven't had the procedure. This led some researchers to think that VSG would also benefit future children, Grayson said. Children born to obese mothers are more likely to be obese themselves and develop high blood pressure and type 2 diabetes.
During her post-doctoral fellowship at the University of Cincinnati, Grayson tested this idea. What she found was quite different.
According to her 2013 study published in Science Translational Medicine, rat pups born to VSG mothers were shorter and lighter than controls, a condition known as intrauterine growth restriction. Pups whose mothers ate high-fat diets after surgery also had high levels of fats and cholesterol in their systems. Grayson compares this scenario to patients who return to “bad habits” post-surgery, like eating high-fat foods instead of the lower-fat diet physicians recommend after VSG.
As adults, these same offspring had more body fat and reduced glucose tolerance, which represent obesity and diabetes in humans.
“We're improving the mom's health, but it's leading to poor outcomes for her offspring,” Grayson said. “No one knew about these effects before the research came out.”

Reckelhoff
Dr. Jane Reckelhoff, Billy S. Guyton Distinguished Professor of physiology and biophysics and Director of the UMMC Women's Health Research Center, says recent studies show similar effects in humans. Children born after their mother's weight-loss surgery were smaller and at increased risk for stillbirth and premature birth, similar to the rats.
“Low birth weight babies face lots of health risks later in life,” Reckelhoff said, including higher rates of developmental disorders.
However, there are no human clinical studies linking a mother's VSG to her children's long-term metabolic health. Bariatric surgery is relatively new and such a study would take several years to complete.
Grayson and other researchers don't know why the VSG rat offspring are smaller and more likely to develop obesity and diabetes. That's the focus of her current research, which she presented in November.
Grayson showed that the VSG mothers had an abnormal, more permeable placenta. She thinks this is an important clue. With higher permeability, everything can pass from mother to baby more easily, she said. That could include hormones, proteins, or microorganisms, but it is too early to know what causes the health problems Grayson sees in her rats.
The VSG moms also expressed more genes that code for inflammation as well as cell death. This starts to answer another finding. VSG mothers have smaller litters and higher resorption rates - their pups die in the womb before fully developed.
The APS conference where Grayson presented her work was sponsored by UMMC's Women's Health Research Center. Reckelhoff, who also serves as APS president, said that other researchers at the conference were very interested in the work and that it is relevant to women considering VSG.
“Younger women are getting bariatric surgery more often than before,” said Reckelhoff. “It's an issue women should know about before trying to become pregnant.”
Vick says Grayson's findings could help improve patient care.
“The more we know the better we can counsel patients on risks and expectations, which I believe leads to improved outcomes.”


