Sharing the pain: Students from four disciplines simulate patient care
In the School of Medicine’s examining room 11, a woman grimaces as she describes a “searing” sensation in her back that “just kills me whenever I sneeze.” Her name: Blaine Penner.
Two doors down, in room 13, a man repeats the complaint. His name: Blaine Penner. In fact, at the University of Mississippi Medical Center’s Judith Gore Gearhart Clinical Skills Center, in separate rooms, Blaine Penner after Blaine Penner is telling the same story at the same time.
But the real story is not this apparent swarm of “Penners,” who are, after all, “standardized patients” – actors interpreting an affliction for the edification of students teaming up to relieve Blaine’s pain.
And that’s the story: In the annals of health care education at the Medical Center, this is the first time students from four different schools have pooled their knowledge in a pursuit meant to make them better at working with each other for the sake of their future patients.
“This was a true interprofessional activity,” said Dr. Kathleen Young, assistant professor of family medicine and director of the Clinical Skills Center, the site of last-week’s Interprofessional Education, or IPE, activity on acute pain management.

Conducted Thursday and Friday, the event absorbed more than 430 students from the schools of health-related professions, medicine, nursing and pharmacy.
Practiced in health care classrooms across the country, Interprofessional Education occurs whenever students from at least two professions learn together. The goal is to accustom professionals from various fields to communicating better with each other, resulting in improved patient care.
“Today, I believe, was probably the most meaningful activity the students could participate in, because it involved so many different disciplines,” said Monica White, a School of Nursing instructor.
“It not only gave them an appreciation of what others do, but also a realization of the contributions they make to the medical team.”
Over the years, the IPE sessions at UMMC threw different schools into the mix, but not until last year did medical students take part – as observers. This time, they suited up as full members of the interprofessional teams, Young said.
“It’s really cool to get everyone’s perspective on how to care for the patient and to hear them come up with some things I may not have thought of,” said Reid Black, a second-year medical student.

SPs are vital for this training and, for years at UMMC, they have regaled learners with their symptoms on examining tables at the Clinical Skills Center, an academic unit of Interprofessional Simulation Training, Assessment, Research and Safety. Formerly located in the Jackson Medical Mall, the center moved to the School of Medicine after the Medical Education building opened in 2017.
“This facility, with its accommodations and technology, makes a world of difference to me as a faculty member, and I’m sure it does for the students as well,” White said.
During last week’s IPE activity, in more than a dozen different rooms, those students dove into the waters of acute pain management to try and bring the “patient” safely to shore. Randall Bolden of Madison channeled patient Penner in room 13.
“We all have scripts,” Bolden said, following his act. “I started training for this two weeks ago.”
In room 11, Dr. Brenda Sumrall Smith, a retired UMMC director of social work and a long-time SP veteran, became Penner.
She gave a convincing performance during a sequence of patient “handoffs” to students – the hospital equivalent of a rash of last-minute laterals in a football game, only slower and minus the desperation.
In between sighs and moans, Penner/Smith revealed details of her acute pain – that is, pain that comes on suddenly, possibly from an injury, as opposed to chronic, which persists for weeks or months because of an underlying condition.
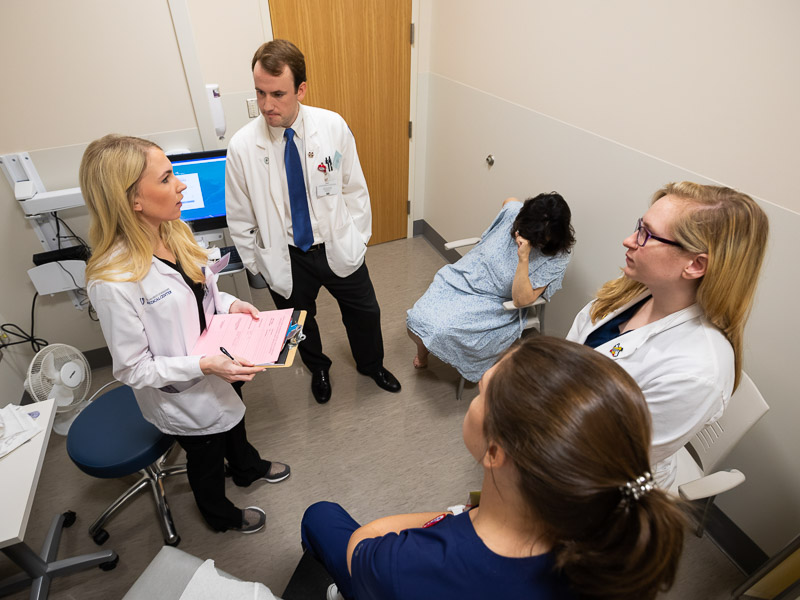
Recording the patient’s family history, prescription information and more in one-on-one encounters were Madison Quinn, nursing; Alyssa Reid, pharmacy; Ben Matthews, medicine; and Emily McDermott, physical therapy.
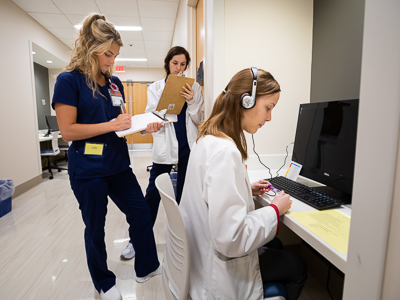
At one of the computer stations lining the hallway outside the rooms, medical student and observer Lydia Nunes, the team’s fifth member, monitored these consultations. From a closed-circuit screen, she watched as the patient, prodded by student questioning, gave up more and more clues with each visit until, at last, the learners got together to compare notes and finger the culprit.
“A bulging disc,” most likely herniated, was the verdict agreed upon by McDermott, the PT, and medical student Matthews. Reid, pharmacy, proposed a seven-day supply of medication to reduce the pain and get Penner back to her job lifting packages for a florist.
Each student weighed in with more recommendations: an MRI, X-rays, a walker, strength exercises, a substance abuse panel, ice treatments, follow-up appointments and more.
“I’m glad to hear that someone is going to write all this down for me,” Penner/Smith said during the team’s presentation to her.
In room after room, a similar scenario played out, until the pretense was dropped and each actor had his or her say.
“You did a good job of showing sympathy,” Smith told the students. “I liked the way you all talked together.”
She did offer some tips: “I wish that you had introduced yourselves using your first and last names,” she said. “And I would have felt more comfortable if you had sat down instead of standing up the entire time.”

Faculty feedback followed. “It was particularly nice that the medical student and pharmacy student got along,” said Dr. Robert Brodell, chair of dermatology. “You seemed to be considerate of each other. You all seemed to enjoy working with other.”
In April, they will have a chance to see if they still do, in a follow-up session that, in IPE world, allegedly takes place six months later, Young said.
“This time the pain will be chronic instead of acute,” she said.
IPE activities, like the pain in Penner’s back, are only going to spread. “Next year, this will be a three-part event that will feature an opioid problem,” Young said.
What won’t change is the essence of the message nursing instructor White reinforced during a debriefing conference with students: “Repeat after me,” she said. “‘I’m an important part of this team and what I have to say can change this patient’s life.’”


