When is an antibiotic the right medicine? New team giving advice
The enthusiasm for the University of Mississippi Medical Center’s efforts to curb misuse of antibiotics is infectious – but in a very good way.
Since being recruited in 2011 to become the new medical director for antimicrobial stewardship, Dr. Jason Parham has built an initiative that promotes antibiotic use “through getting the right diagnosis, the right drug, the right dose, the right route and the right duration,” he said. “Most importantly, antimicrobial stewardship programs (ASP) are about doing the right thing for patients.”
Flash forward to 2018, and ASP is taking the next leap. Parham, associate professor of infectious diseases, has expanded his team to better address the problem of antibiotic overuse in the ICUs, Batson Children’s Hospital, and outpatient clinics. Until now, ASP has focused primarily on patients in University Hospital because of the high volume of antibiotics prescribed there.
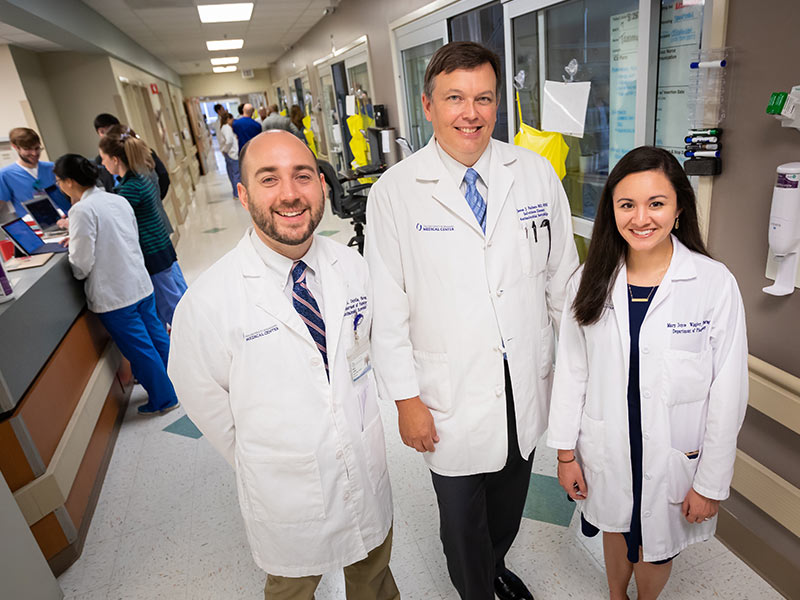
Dr. Mary Joyce Wingler, who recently completed an infectious diseases residency with the School of Pharmacy, began working for UMMC’s ASP in August. She joins Dr. David Cretella, hired in 2015 as the Medical Center's first antimicrobial stewardship pharmacist. Cretella also completed a pharmacy residency in infectious diseases at UMMC.
The trio work together to scrutinize antibiotics prescribed to inpatients with an eye for their appropriateness – and if they see a need, to recommend to the patient’s provider tweaks in dosage or drug, or its delivery via mouth or IV. “The three of us collaborate to come up with a vision of how we want to improve antimicrobial use and the quality of care delivered at UMMC,” Parham said.
“David is an excellent stewardship pharmacist and a sharp mind,” Parham said. “Before David was hired, whenever clinical duties pulled me away from stewardship, the number and depth of interventions suffered as we cobbled together volunteer support to fill in the gaps.
“Mary Joyce is a fantastic addition to our program. She was a calm, insightful presence throughout her training,” Parham said. “She showed exceptional initiative in audit and feedback on patients in Children’s and antiretroviral stewardship in our HIV-positive patients.”
Antibiotic stewardship is Parham’s mission, driven by the fact that the misuse of antibiotics is one of the nation’s most pressing public health challenges. Not only can inappropriate use of antibiotics build resistance to those drugs when they’re most needed, but the patient can suffer unnecessary adverse effects such as nausea, gastrointestinal distress and skin irritation, among others.
The problems are caused when a provider prescribes an antibiotic for a virus instead of a bacterial infection, or prescribes a strong antibiotic when a less powerful or more narrow-spectrum one is most appropriate. Or, the provider prescribes a long course of an antibiotic when a shorter duration is most appropriate.

Parham and his team quietly work behind the scenes, reviewing thousands of charts of inpatients who are on some form of antibiotics. “Our message to providers is simple: using antibiotics wisely is difficult. We can help,” Parham said.
The three use a clinical surveillance software program to set parameters for selecting patients needing scrutiny. “We have patients who are reviewed because they are on restricted antibiotics, or patients who are on a certain antibiotic for three or more days, or who are on three or more antibiotics,” Parham said. “We review all blood cultures that come back positive for an infection. We might have 600 patients in the hospital on a given day, but only 30 to 40 patients that day meet the screening criteria.”
In about 20 percent of charts flagged for reviews, the team makes a recommendation to the provider on how to better optimize use of an antibiotic. Recommendations are delivered via open communication with a variety of physicians, nurses and nurse practitioners. “About half of the inpatient antibiotic use is in the hospital, another 20-30 percent in the ICU tower, and another 20 percent in the pediatric hospital,” Cretella said.
Team members also round with fellows in the ICU. “It’s a more personal approach,” Cretella said. “It‘s a forum for them to ask questions, and for us to pass on recommendations.”
“It’s been a great process for us,” said Dr. Demondes Haynes, professor of medicine in the Division of Pulmonary and Critical Care Medicine. “In the ICU, we have a ton of patients, and there are a lot of infections that we manage. Sometimes, they pick up something that we’ve overlooked, or they might say, ‘You’re covering the right organism, but have you considered a more narrow-spectrum antibiotic?’ Making that change can decrease resistance and sometimes decrease costs.”
It’s that face-to-face interaction that builds a trusting relationship that allows frank discussion. “A lot of times, people think that they (the ASP team) tell you what you have to do. They don’t,” Haynes said. “They help us continuously to learn, and when we tell them what we were thinking about a patient, it’s very educational.”
“Everything we do is patient-centered,” Wingler said. “We evaluate them through their charts, and we talk to the physicians who actually see them. We might say: ‘It looks like the patient is improving. How does the patient look today, from your perspective?’
“The physicians are always willing to talk about their patients. That’s been excellent.”
The intimate look at patient charts gives the ASP team unique opportunities to partner with providers on prompt care. “One of the biggest places we can have an impact is following up on blood cultures,” Wingler said. “We’ve seen a positive blood culture come up on a chart before the provider has seen it. We can recommend an antibiotic for the patient, and they start getting better immediately.”
ASP has achieved concrete results at UMMC, Parham said. In a comparison of antimicrobial use rates in University Hospital during 2012 versus 2017, piperacillin-tazobactam use is down 22%, azithromycin is down 34%, vancomycin is down 50%, levofloxacin is down 53% and linezolid is down 85%.
“It’s appropriate to use a broad-spectrum antibiotic before we know what’s going on with the patient,” Parham said. “Once two or three days have passed, we recommend that the provider take an antibiotic time out to see how the patient is improving, and to see what the cultures and other clinical data are suggesting.
“Often, they can narrow the antibiotic down to target the organism more effectively and get the patient off the broad-spectrum antibiotic – or if it’s not an infection, stop the antibiotic.”
In the works is additional provider education on antibiotic use. “This coming year, we will see an active collaboration with the Department of Family Medicine to optimize prescribing practices in their clinic locations. Having two well-trained, energetic stewardship pharmacists is going to yield amazing results,” Parham said.
“We want to do anything that we can do to encourage good prescribing, but to give physicians the ultimate choice,” Cretella said. “We are very big on that. We’re about empowering and supporting physicians to make good choices.”


