
UMMC’s sophisticated lab identifies most baffling opioids, street drugs
By: Ruth Cummins
When a Mississippi law enforcement agency is stumped about what deadly substances are laced into a street drug they've confiscated, there's only one hospital laboratory in the state that has the tools to figure out the most puzzling cases.
The University of Mississippi Medical Center's analytical toxicology laboratory uses sophisticated equipment and testing methods to scrutinize blood and urine samples in addition to samples of illegal "designer" drugs and prescription medicines. Their work helps identify what dangerous street drugs are making the rounds in the state and what trends to expect in the future.
The Medical Center's laboratory work and its outreach efforts to educate and empower the medical community are impacting the face of opioid abuse in Mississippi. Of the 563 drug overdose deaths in the state since 2013, 481, or 85 percent, were opioid related, said John Dowdy, director of the Mississippi Bureau of Narcotics.
"You may have no clue what you're buying on the street," said Lee Spencer, lead technician in the toxicology lab. "That's why there's so much attention on opioids now. People are buying alphabet soup, and they don't know what's in it."
In Mississippi, opioids such as morphine, oxycodone and hydrocodone are commonly prescribed for pain, and commonly diverted for use by addicts or for illegal sale. But it's the synthetic and semi-synthetic forms of opioids, producing the same feeling of euphoria, that are causing the death toll to rise. They're easier to obtain, and many are manufactured in Asia to be sold recreationally. One of the most popular, fentanyl, is 50 to 100 times stronger than morphine.
"Some of the derivatives of fentanyl - alfentanil, sufentanil, carfentanil - are 100 to 1,000 times more potent than morphine," said Dr. Patrick Kyle, a toxicologist and associate professor of pathology.
"That's what people are dying from. It's very easy for an individual to overdose," said Kyle, who leads a team of five technicians in the laboratory that analyzes up to 8,000 samples a month.
UMMC uses an arsenal of specialized equipment that includes mass spectrometers, which analyze and give a picture of the chemical composition of a blood or urine sample based on their mass and molecular fragments. It's often partnered with chromatography, which analyzes both gases and liquids. UMMC houses the only hospital laboratory in the state with a mass spectrometer.
Place a small vial of blood or urine in the mass spectrometer, and it will tell you what traditional or synthetic opioid has been ingested, how much and in what concentration. It also analyzes samples of many other prescription or street opiates, plus often-abused drugs including cocaine, synthetic cannabinoids such as spice, as well as amphetamines and other attention deficit disorder meds.
When UMMC's mass spectrometer was purchased, Kyle said, he and his staff worked for two to three months to develop its array of testing. "It arrives unprogrammed," he said. "We inject chemical standards and program the analyzer to the drugs we're seeing, or expect to see, in Mississippi. We monitor the news reports and stay in close touch with law enforcement. It's very hands on, and very labor intensive."
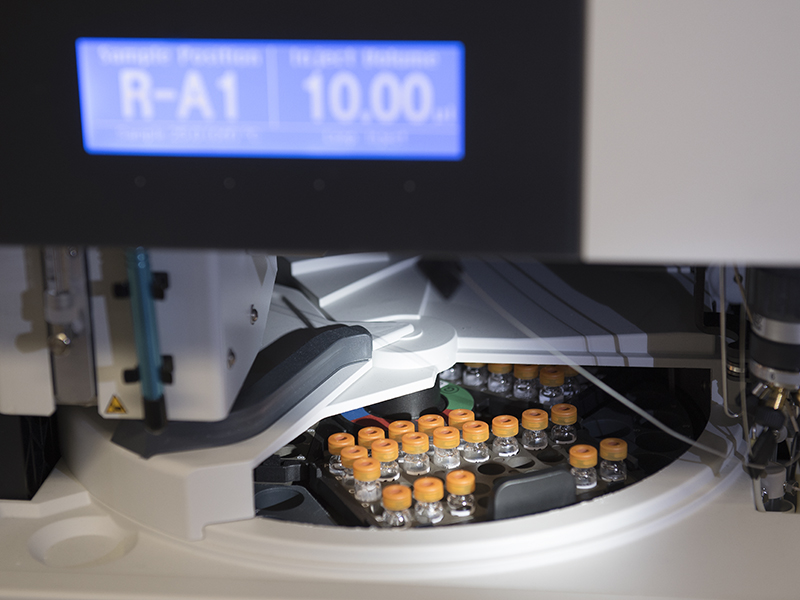
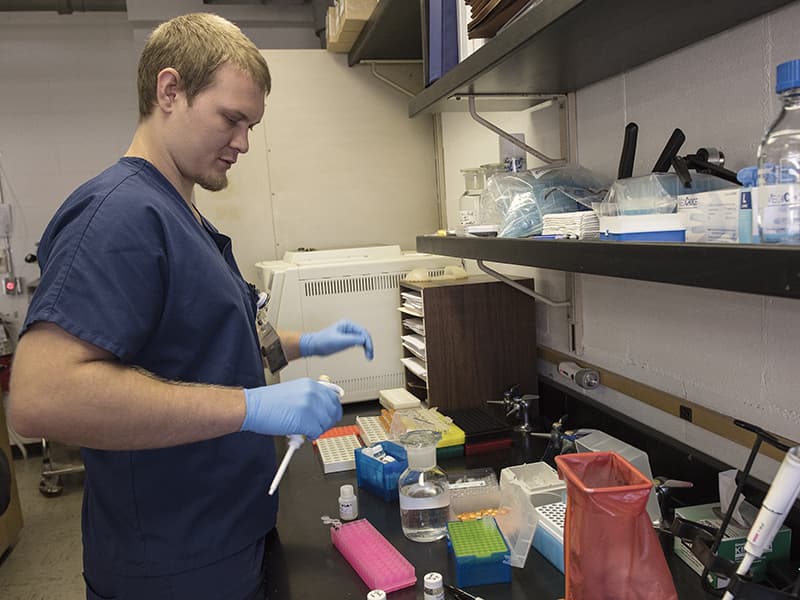
Techs even test the instrument to see how well it tests. Lab technician Derek Johnson recently used prescription opiates in a solution to validate whether the instrument was detecting the drugs and their synthetic versions in urine at very low concentrations. "It can pick up 25 nanograms (one billionth of a gram) per milliliter of urine," Johnson said.
There's no typical day in the toxicology lab. "One phone call can change everything," Spencer said.
It could be from a law enforcement agency or UMMC's Emergency Department alerting the team to an influx of spice overdoses, or a heads' up about a particularly toxic "designer" batch of synthetic opioids from Asia making inroads into Mississippi. The team also analyzes specimens from children and babies, not just adults. Recently, the team found the powerful muscle relaxer cyclobenzaprine in the blood of a child brought to UMMC, and it's not unusual for them to test the blood of a newborn after the baby and its mother fail an initial screen for opioids.
"Sometimes, it's a small child who finds a tablet on the floor and ingests it," Spencer said. "A 3-year-old can't tell the difference between a tablet and a Skittle."
UMMC has the only clinical laboratory in the state that can analyze for ethylene glycol and methanol poisoning, which happens when someone ingests antifreeze or high-proof "moonshine" alcohols manufactured illegally, said Dr. Robert Cox, professor of emergency medicine and director of the Mississippi Poison Control Center based at the Medical Center.
"We can call them (the laboratory techs), even if it's at night, and they will give us an answer. That's a big thing," he said. "If someone calls us from Meridian, they send a blood sample over here and get an answer in a day. If any hospital in the state doesn't want to do that and instead send it out of state, they'll get an answer in three days."
The laboratory has a technician on duty around the clock to analyze body fluids or samples of drugs or other toxic substances as requested. "It is a valuable resource to have available 24/7, and their team has always been more than accommodating to the ED in order to meet our needs to be able to take care of that population of patients," said Jason Zimmerman, a registered nurse and director of the Medical Center's nursing adult services.
Of the 200-plus drug overdose deaths in the state in 2016, the majority were combinations of heroin, opioids, or synthetic opioids such as Fentanyl, Dowdy said. "Your typical street drug such as black tar heroin or methamphetamine ice or powder cocaine we can usually identify on sight," he said. "But when we start getting into the synthetic realm, that's when what UMMC does is so critical."
When hundreds of Mississippians overdosed on spice in a single spate a couple of years ago, he said. "there was a strand that we found that no one knew what it was. UMMC was the only place that could identify it for us."
"People here are primarily using prescription opioids" to achieve a euphoric high, Kyle said. "The monitoring of pain management patients is lagging in Mississippi so far as screening and detection. We seem to be five to 10 years behind the rest of the country."
And although law enforcement agencies are conducting drug roundups and taking dozens into custody, Kyle said, "we still have pill mills here, and doctors who haven’t been busted. They say "Give me $60, and I'll give you a prescription."
The amount of opioids prescribed in this country was three times higher in 2015 than in 1999, according to the federal Centers for Disease Control and Prevention. Mississippi is a leading prescriber of opioid painkillers, with the equivalent of 70 opioid pills for every man, woman and child in 2016 – placing the state fifth highest per capita in the nation, with 1.07 prescriptions per person, the state Department of Mental Health says.
In Mississippi, Kyle and Spencer say, the abuse of opioids knows no particular city or rural hamlet, race, age, sex or education level. And not just users, but law enforcement officers who handle confiscated drugs are at risk, he said. Kyle cited a recent incident where an Ohio officer was exposed to fentanyl in a white powder form during the course of a drug bust. “The officer noticed some on his uniform and brushed it away with his hand, then fell on the ground a few minutes later,” Kyle said. “The amount absorbed through his skin was enough to send him to the hospital.
“We run the same risk in our lab as samples are received,” he said.
Kyle and his technicians consider it part of their mission to educate the medical and law enforcement communities about opioids that they’re seeing. They’ve created a semi-annual newsletter, Mississippi Toxicology Bulletin, delivered to hospitals and law enforcement that aims to increase awareness of what the state should expect.
They share information on the lab’s work and their findings by setting up a table at meetings and conferences, including the July 11-13 Opioid and Heroin Mississippi Drug Summit sponsored in part by the office of Attorney General Jim Hood and the Department of Mental Health.
Most opioid use in Mississippi is by those 40 and younger, Kyle said, and people in Mississippi who abuse opioids and die most often have ingested hydrocodone or oxycodone. Right now, Mississippi isn’t gripped in the larger scope of the synthetic opioid crisis seen in other parts of the country, he said, but it’s increasing, and it’s a matter of time.
What that could look like – and what it looks like in Ohio and other states hit hard: “You’ve got mom and dad on the side of the road in their vehicle, with children inside, and mom and dad are totally unresponsive,” Kyle said.
“We’re seeing some abuse of heroin, but not like in the bigger cities. But it’s coming, and it’s very dangerous. Mixing the fentanyls with heroin increases the danger, because they are much stronger than heroin.”


