Precision med new avenue for brain, nervous system treatment
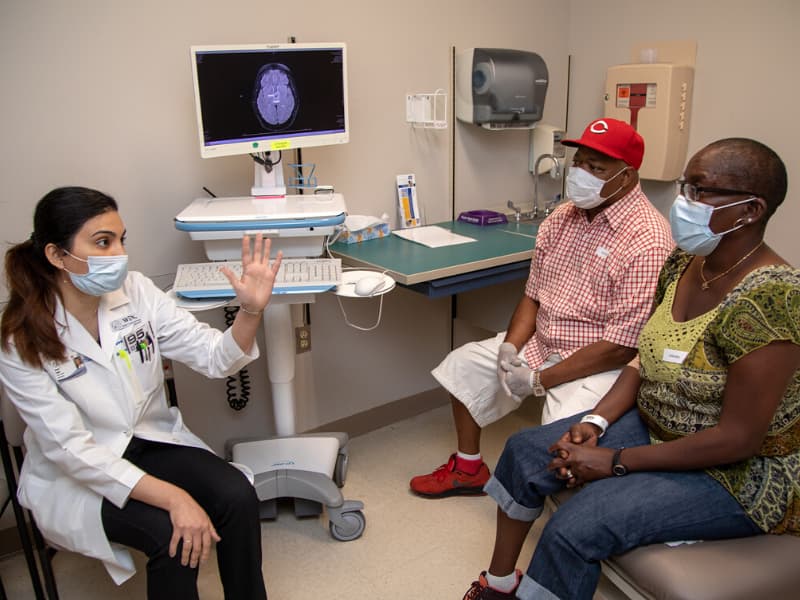
Within days of discovering she had a brain tumor, Marzina Jones of Jackson embarked on a journey that led to a treatment tailored precisely for her.
The University of Mississippi Medical Center team that treats malignant and non-malignant brain tumors completed a biopsy and diagnosed Jones with a rare ganglioglioma with a BRAF mutation.
Dr. Nawal Shaikh, a neuro-oncologist with the UMMC Cancer Center and Research Institute Interdisciplinary Brain and Central Nervous System Tumor Program, said the technology used to confirm the specific mutation “has only been available in medicine for a few years.”
Because of the tumor’s location, doctors did not recommend surgery or radiation therapy, telling Jones those therapies might leave her paralyzed on her right side. “I didn’t want that,” she said.
The targeted therapy Jones receives hones in on the BRAF mutation in the cancer cell. It’s part of precision medicine, a growing field in cancer therapy that includes looking for mutations in cancer cells that happen for no known reason and those that are inherited.
In neuro-oncology, CCRI providers are using a broad spectrum, next-generation sequencing platform to examine the DNA properties of brain and central nervous system tumors. That means they look for multiple known mutations.
“I offer it to every single patient, whether it is a brain metastasis or primary brain tumor,” Shaikh said of the testing. Results give physicians insight into a tumor’s molecular and genetic makeup and indirectly into tumor biology.
“You’re trying to create the best treatment plan for the patient and not a cookie cutter treatment plan,” said Shaikh, a UMMC assistant professor of neurology. “Hopefully, this dissolves that tumor or impedes its growth.”
Knowing a tumor’s genetic makeup also helps providers rule out medications that are unlikely to help, thus more quickly selecting a therapy that will work, she said.
While helping determine optimal treatment, Shaikh said testing also can provide information on how aggressive a tumor may be.
“If you find a lot of mutations, the provider should be aggressive from the get-go,” she said.
Finding particular mutations also may allow doctors to use off-label therapies – drugs approved for use in other cancers with the same mutation but not yet offered as a standard of care for brain tumors.
Using DNA testing may provide team members with information on DNA mutations that were inherited. In that case, according to Dr. Joseph Maher, head of the Division of Medical Genetics and Precision Medicine at UMMC, a patient’s relatives can be tested for the mutation and, if they have it, a schedule of regular, possibly annual, neurological exams can be worked out to try to discover any brain tumor early.
Maher uses Lynch Syndrome as an example. The disease, known to increase the risk of colon cancer, also increases the risk of certain brain tumors, but to a lesser degree.
Unlike colon cancer, where doctors know to recommend patients start screening earlier and more often, researchers are still trying to discover how and how often to screen for brain cancers, said Maher, a geneticist who works with several UMMC CCRI programs.
Dr. Mark Anderson, a neuro-oncologist who heads the UMMC Brain/CNS Program, said while a patient may not know he or she has a brain tumor until symptoms are exhibited, knowledge of a possible inherited trait can help better interpret symptoms when they do occur. Anderson added that based on current knowledge, the lifetime risk of developing brain tumors is about 2 percent: It’s four times higher for those with Lynch Syndrome.
“There are no screening guidelines that tell you what to do,” said Anderson, a UMMC associate professor of neurology. “The general recommendations we follow are to recommend yearly neurological examinations and investigate any symptoms as they develop.”
The team also may recommend a baseline MRI, or magnetic resonance imaging, so it will have images to compare if symptoms show up years later.
Anderson said one day, he expects cancers to be treated based on the mutation within the cells instead of the part of the body where the cancer started. He said he also knows the human brain protects itself and some drugs that may work on a breast cancer would have trouble crossing the blood-brain barrier. Researchers, including some at the UMMC CCRI, are working to overcome those delivery obstacles.
Even the targeted therapies available now may take time to show changes in the tumor, he said.
“If they’re targeting slower-growing tumors, it takes a longer time to see shrinkage in brain tumors,” Anderson said. “Tumor cells may be dying, but it’s harder to see dead cells versus live ones.”
That’s stressful for patients “because they have a sensation there’s something there.”
The stress started on Thanksgiving Day for Jones.
“We were watching football and I ended up on the floor,” she said. “I woke up and asked my husband, ‘What am I doing here?’”
His reply: “You passed out.”
By Dec. 4, her doctors had discovered the brain tumor and sent her to Dr. Roberto Rey-Dios, a neurosurgeon in the UMMC Brain/CNS Program. A biopsy and pathology testing confirmed the diagnosis and genetic testing confirmed the mutation.
Jones said she misses her work at a deli on Fortification Street and hopes to return one day. She and her family also live within the confinements of COVID-19 and her doctors’ requests that she not drive.
For now, Shaikh said they are continuing treatment and monitoring the tumor’s status with imaging. So far, it appears to be stable.
The above article appears in CONSULT, UMMC’s monthly e-newsletter sharing news about cutting-edge clinical and health science education advances and innovative biomedical research at the Medical Center and giving you tips and suggestions on how you and the people you love can live a healthier life. Click here and enter your email address to receive CONSULT free of charge. You may cancel at any time.



