Why UMMC blood bank staff call state’s response critical during COVID-19 outbreak
When tragedy strikes, Mississippians give.
That proved true last month as COVID-19 spread across the country, cancelling events throughout the state, including blood drives.
As available blood levels reached critical stages, the pleas began and hundreds turned out to bleed life for their fellow Mississippians.
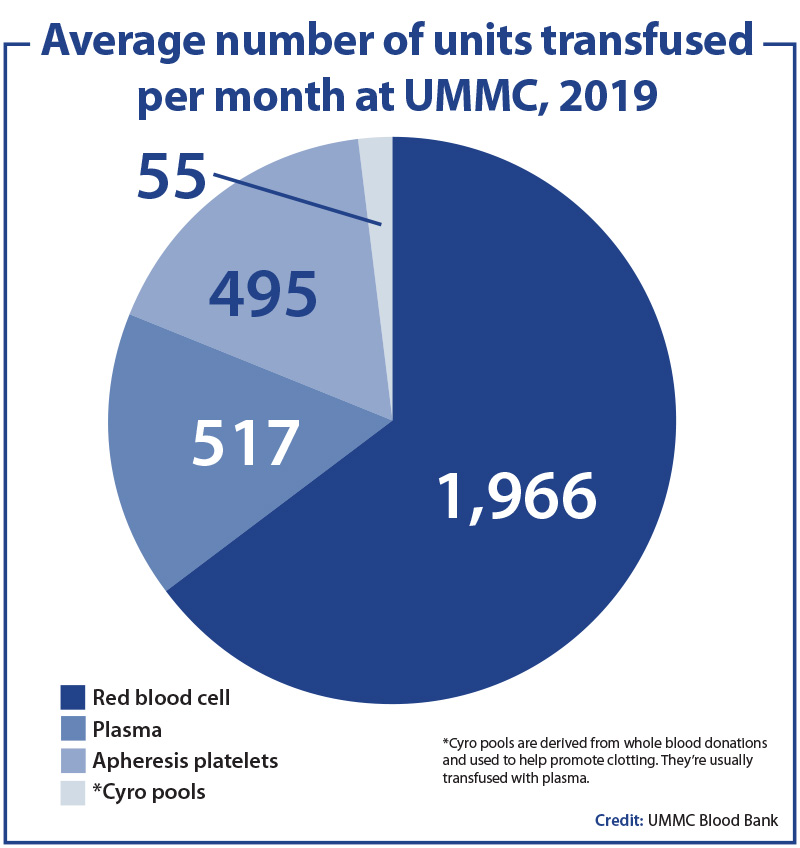 The issue hit home with the University of Mississippi Medical Center’s Blood Bank, where staff monitor, receive and deliver an average of about 3,000 blood or blood products for transfusion each month.
The issue hit home with the University of Mississippi Medical Center’s Blood Bank, where staff monitor, receive and deliver an average of about 3,000 blood or blood products for transfusion each month.
Uses range from the expected - trauma and surgical patients - to the sometimes unknown - NICU babies, who may need only small portions of a donation to survive.

Dr. Sara Johnston, who directs the blood bank, said this shortage was more significant and scary.
“When disaster happens, if there’s a tornado here or they have flooding in the Northeast, you can bring blood in from other parts of the country and people will step up and donate,” said Johnston, a UMMC assistant professor of pathology. “With COVID-19, you can’t pull from another region.
“Blood drives across the country are getting cancelled. That’s why it’s so important for people locally to give.”
 At Mississippi Blood Services, the state’s donation organization, officials are doing all they can to minimize the COVID-19 threat for donors. Donation buses are limited to no more than 10 people, meaning those who usually handle up to four donors and two prospective donors in screenings have cut back to only two donors and two in screening at any time. Those working in the main stations are consistently sanitizing offices and donor spaces.
At Mississippi Blood Services, the state’s donation organization, officials are doing all they can to minimize the COVID-19 threat for donors. Donation buses are limited to no more than 10 people, meaning those who usually handle up to four donors and two prospective donors in screenings have cut back to only two donors and two in screening at any time. Those working in the main stations are consistently sanitizing offices and donor spaces.
Johnston said it is unlikely any patients receiving blood will get COVID-19 from a donor who may not have known he or she had the novel coronavirus.
“Respiratory viruses have never been shown to be transmitted through blood transfusions,” Johnston said. To be safe, she said blood donors are screened for symptoms of COVID-19, as well as dozens of other conditions that could knock them out of the donor pool.
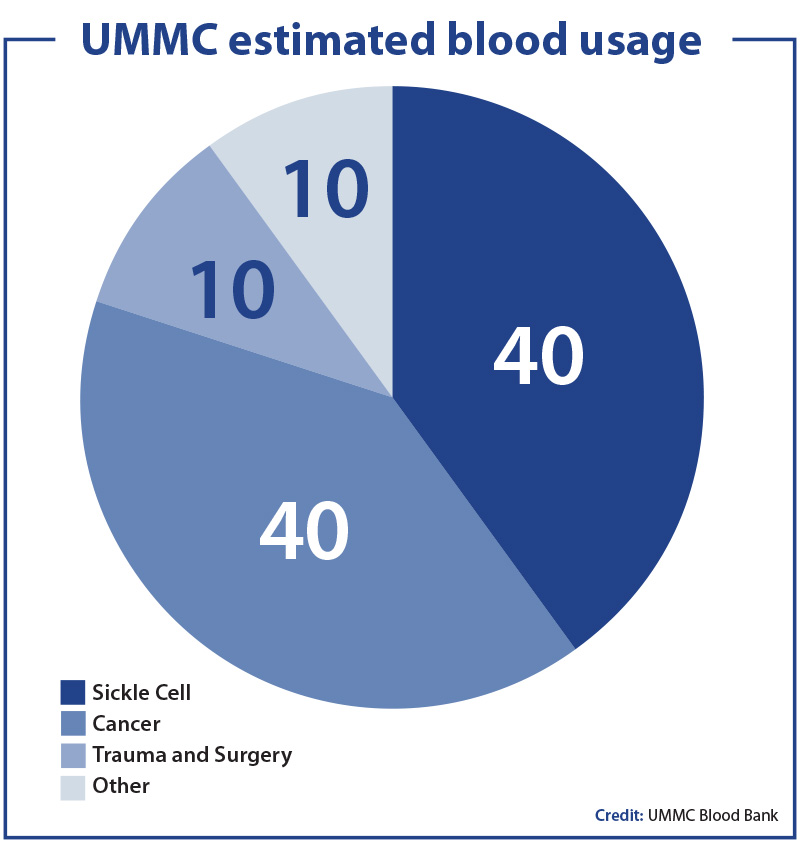
So just how is the blood used?
Hope Blanton, a lab services manager, said usage may vary day to day and usually includes:
• Trauma and surgery.
Patients brought to the emergency room with injuries may need blood quickly. Initially, that may mean Type 0-positive and Type 0-negative donations. O-negative is a universal donor. Once the blood bank can test for blood type, it switches to a match for the recipient.
“The problem with trauma is, if you have one patient who has very bad bleeding after a car accident or gunshot wound, we can use 100 units in a matter of minutes,” said Dr. Matt Kutcher, a UMMC assistant professor of surgery. “That can be lifesaving, but we can never anticipate it.”
In those situations, there is no opportunity to call for donors, so the blood has to be available in the UMMC blood bank. Kutcher described one recent two-week period: “We needed a large amount of blood very quickly, maybe 50 units per person for two people.”
While elective surgeries have been postponed for now, some surgeries requiring blood, such as cardiac and vascular surgeries, have to continue, he said.
• Cancer patients.
“Many of our blood cancers result in the need for transfusions and many of our treatments increase that need as well,” said Dr. Stephanie Elkins, head of the Division of Hematology and Oncology, a part of the UMMC Cancer Center and Research Institute. “The majority of our patients with acute leukemia and those requiring special treatments, such as marrow transplants, require multiple transfusions of both red cells and platelets during their treatment course.
“Without the blood donations from our donors, many of our patients would die during therapy from low counts.”
The intense cancer treatments given to children have increased survival to more than 70 percent for pediatric cancers today. Dr. Anderson Collier, who heads the Children's of Mississippi Center for Cancer and Blood Disorders, said such treatments must be supported by blood and plasma transfusions.
“Either the intensity of our therapy will have to decrease and thus decrease survival of kids with cancer, or children will die from the toxicities of their therapy,” Collier said.
• Non-malignant blood disorders, including sickle cell.
“One of the devastating consequences of sickle cell disease in children is strokes,” said Collier, a UMMC professor of pediatric hematology and oncology. “We now screen patients with ultrasound to determine their risk. The only proven treatment to prevent kids from having a stroke or to keep kids from having another stroke is chronic blood transfusions.
“This treatment keeps the amount of sickled blood low so that the stroke risk likewise stays low.”
He said each child at risk may need one to three units of blood a month.
“Without these transfusions, more children will have to live with the lifelong consequences of a stroke and some will die from it,” Collier said.
Children and adults with other red blood cell disorders that cause lifelong anemia will need transfusions during times of illness, too, he said.
“They need blood transfusions to save their lives.”
• Other needs, including a wide range from infants in the Neonatal Intensive Care Unit to women who hemorrhage while giving birth.
Just as the demand for blood rises, so does the need to properly handle and use it. Blanton said once the blood bank receives blood, staff test to confirm the blood type – A, B, AB or O – and whether it is positive or negative, the Rh type.
When an emergency is not involved, blood bank staff are able to test a patient for blood type, Rh type and for any antibodies he or she may have.
People may acquire antibodies if they have received a blood donation or had a child. This means they have received blood other than their own and their bodies may form antibodies to reject the donor blood. In those cases, staff look for donated blood without the antigens that would prompt those antibodies to react.
“Once that’s done, we put it on the shelf in order by day it was received and blood type,” Blanton said. “It’s only good for 42 days, so we want to use the units that are going to expire soon first.”

Hope Blanton, UMMC Blood Bank lab manager.
When they receive an order for blood, blood bank staff search for the correct ABO and Rh type, then for antigens that may harm that patient.
“We have a lot of sickle cell and cancer patients,” Blanton said. “These patients tend to have lots of antibodies because they’ve been transfused a lot.”
If the needed product isn’t on the shelves, Blanton starts a regional search for it. Sometimes, especially for sickle cell patients, that may take days and has involved calls nationwide. Whenever possible, hematologic and cancer staff work with the lab to let the staff know in advance when patients who need blood will arrive.
Before the COVID-19 pandemic, the U.S. Food and Drug Administration and the American Association of Blood Banks outlined a process to identify whether measures other than transfusion could handle a medical need. That has become even more important now, Blanton said.
Kutcher said physicians are looking for options other than blood.
“In trauma, we may use clotting factors that don’t come from blood early on to try to conserve blood.”
“In general, you never have enough blood,” Blanton said.
Since less than 40 percent of the U.S. population can donate blood, it is important that those who can donate, said Johnston.
“We don’t know how long COVID-19 and shelter-in-place will continue,” she said. “It’s important for people to not necessarily donate this week, but to come out a month from now.
“If this continues for months and months, we need people to still be enthusiastic about donating.”
For more information about donating blood, check with Mississippi Blood Services at www.msblood.com or call 1-888-90-BLOOD.
The above article appears in CONSULT, UMMC’s monthly e-newsletter sharing news about cutting-edge clinical and health science education advances and innovative biomedical research at the Medical Center and giving you tips and suggestions on how you and the people you love can live a healthier life. Click here and enter your email address to receive CONSULT free of charge. You may cancel at any time.



