Come What May, We'll be Ready
Good morning!
Last week I alluded to the fact that we were ready to receive patients evacuated from the Houston area in the aftermath of Hurricane Harvey, had that become necessary.
This week we are watching as Hurricane Irma devastates the Caribbean and makes its way toward Florida. The forecast models do not show Irma heading into the Gulf, but if it did come our direction, I know we would be ready.
What has made us ready for these extreme weather events was what happened just about 12 years ago after another hurricane, Katrina, devastated New Orleans and the Gulf Coast.
 Before Hurricane Katrina, UMMC did not have a formal statewide role in disaster response. Our experience in major medical emergencies had been primarily to react, receive patients from elsewhere and assist around the margins as needed.
Before Hurricane Katrina, UMMC did not have a formal statewide role in disaster response. Our experience in major medical emergencies had been primarily to react, receive patients from elsewhere and assist around the margins as needed.
After Katrina, we completely overhauled our emergency response capability to be more proactive, more forward leaning, so today, UMMC is able to play a leading role in statewide disaster medical response.
This change in our role was the result of a deliberate decision on our part because, frankly, we didn’t like the feeling of being underprepared and at the mercy of events when confronted with a crisis.
Let me give you a few examples from Katrina.
The storm devastated the health care infrastructure of the lower third of Mississippi. Hospitals, nursing homes, clinics, ambulance services – most were forced to shut down and evacuate patients by whatever means available.
UMMC was asked by the Mississippi State Department of Health to send personnel to help with the disaster medical response. Although well-intentioned, the best we could muster was a small, seat-of-the-pants operation, especially given the scope of the damage. Even with a well-trained team of six physicians and two nurses, this brave group was woefully ill-equipped to handle the medical need they encountered.
We were also asked to coordinate all out-of-state ambulances and help coordinate patient movement in the affected areas. We did so with sticky notes and a dry-erase board.
Anything we might do for the state was complicated by the fact we had our hands full in the metro area. Although it’s 165 miles inland, Jackson experienced sustained Category 1 hurricane winds, so we were dealing with injuries from car wrecks, fallen trees and swift water rescues, not to mention water and electricity outages and shortages of gasoline and staff.
We received many patients from evacuated coastal hospitals. And we attended to the medical needs of displaced people in shelters. Several hundred evacuees sheltered in the Mississippi Coliseum and we assigned physicians and nurses to assist with their care.
This was heroic work under the most challenging conditions, but it was well short of what we felt was needed in the way of a statewide disaster medical response.
Since Katrina, in cooperation with other state agencies, we have built up our infrastructure and physical assets for response in similar situations. These include:
- three mobile field hospitals
- a mobile ER/ICU
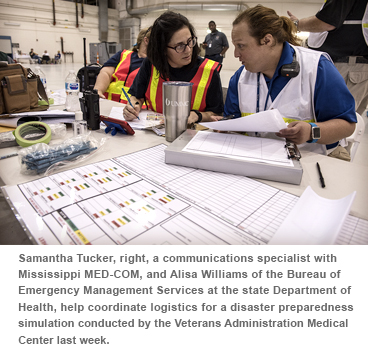
- Mississippi MED-COM, established to serve as a communications hub to coordinate statewide emergency response
- four medical helicopters to transport our expertise to the field rapidly (compared to one during Katrina)
- designation as a primary agency for ESF8 (emergency support function for public health and medical services) for Mississippi
- the UMMC Center for Emergency Services, established to build and operationalize our emergency capabilities, including increased staffing, planning, training and education
- the ability to scale up from a two-person team to a 50-person outreach team, depending on the disaster
This enhanced capability was put to the test after an E4 tornado made a direct hit on the hospital in the town of Louisville in 2014. UMMC was part of the state's coordinated response and sent in several emergency medical teams by ground within an hour of the storm. Our teams supported the hospital staff, triaged and stabilized patients on the scene, and coordinated the evacuation of the hospital and a nursing home. We placed a mobile emergency room in the Walmart parking lot and remained in Louisville for two-and-a-half weeks after the storm to help the Department of Health and MEMA with recovery efforts.
Our role in the state’s disaster response system continues to grow, with exciting plans for a first-responder training center on our campus and continued outreach efforts to rural communities. Leaders of our emergency response team (including Terry McLeod, who I failed to mention last week) work seamlessly with MEMA, the Department of Health, the Mississippi National Guard and federal agencies to safeguard lives when we are faced with these dire emergencies.
Statewide disaster medical response is part of the value UMMC provides to our state that is not always visible or appreciated. Until it is. So while we hope and pray that those in Irma’s path are safe and sound in the hours and days ahead, I’m grateful that when the next disaster strikes Mississippi, all the work that’s been done post-Katrina means we’ll be ready.