|
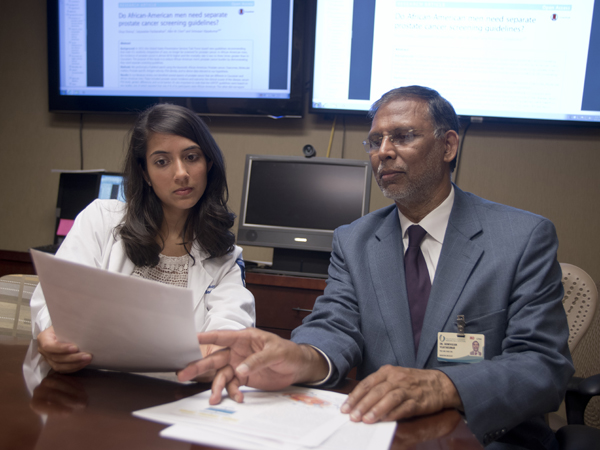
A higher percentage of African-American men die of prostate cancer than males of any race in the nation - an alarming fact for both health-care providers and researchers. That's the impetus for a recommendation by a group of researchers that black men should have their own prostate screening guidelines. “We know a higher percentage of African-American men die of prostate cancer, and they tend to have more aggressive forms of it at the time of initial diagnosis,” said Dr. Srinivasan Vijayakumar, director of the University of Mississippi Medical Center Cancer Institute and Department of Radiation Oncology. “Since deaths from prostate cancer are higher in this population, we think we need separate prostate screening guidelines for African-American men.” In 2012, the leading agency that establishes cancer screening guidelines issued new ones, saying men with no symptoms should no longer be screened for prostate cancer. Today, however, new researchers have found the recommendation is mostly based on two studies that included few black men. Vijayakumar was an author on the paper, published in BioMed Central Urology in May. The research shows: - The incidence of prostate cancer is 60 percent higher in black men than in the U.S. male population as a whole.
- Deaths from prostate cancer are two to three times higher among black men than among caucasian men.
- Black men have more aggressive forms of prostate cancer, tend to have higher prostate-specific antigen (PSA) values, and some research shows may have biological factors that make them more susceptible to prostate cancer.
- Social factors, such as lack of insurance, also may mean black men are less likely to be screened or treated for prostate cancer.
- Multiple groups cite being a black male as a risk factor for prostate cancer.
When the U.S. Preventative Services Task Force issued the new screening guidelines in 2012, it didn't take those differences into consideration, the authors say. “This raises concerns about the reliability of the study for an African-American patient population,” said Divya Shenoy, an author on the paper and third-year medical student at UMMC. That's important in a state like Mississippi, where 40 percent of the population is black. Shenoy said it's worthwhile “to invest in more tailored guidelines that are race-specific, as African-Americans have higher rates of morbidity and mortality due to prostate cancer.” Screening recommendations were largely based on two studies: the Prostate, Lung, Colorectal, and Ovarian Cancer Screening Trial (PLCO) and the European Randomized Study of Screening for Prostate Cancer (ERSPC). The PLCO trial reported 4 percent of the men were non-Hispanic blacks, while the ERSPC study did not report racial demographics. The ERSPC study was conducted in seven European countries with low populations of men of African descent. Prostate screening came under review because many believed too many men were overdiagnosed and overtreated, Vijayakumar said. The U.S. Preventative Services Task Force argued that even prostate cancer that is causing no symptoms may be detected. Many of those cases may not affect a man's overall survival, especially if the prostate cancer is not aggressive. The man is more likely to die of another cause before prostate cancer symptoms start. The review of various studies led the authors to conclude that while prostate screening may lead to overtreatment in the overall group of men, black men who tend to have more aggressive prostate cancers and die from it more frequently, should be screened with traditional and new genetic methods. Even with its pitfalls, PSA has a place in screening. “PSA, while a useful screening tool, is not very specific and can be elevated even when a man does not have cancer,” Shenoy said. “PSA ought to be utilized, but utilization should be patient specific, based on myriad factors such as age, family history, and symptoms. PSA-based parameters such as PSA velocity and PSA density are still important biomarkers and can be helpful tools in diagnosis and treatment of prostate cancer.” Shenoy said the authors also recommended the use of new biomarker tests currently being developed to identify aggressive and non-aggressive prostate cancers. “The common misconception is that all prostate cancers are the same, which is not true,” Shenoy said. “Biomarkers are useful in personalizing medicine to distinguish between aggressive and nonaggressive forms of prostate cancer and would help personalize the diagnoses and then the subsequent treatment. This approach would improve the quality of care patients receive.” While the screening guidelines may be sensible for most U.S. men, the authors propose new guidelines be developed for African-American men. Until that happens, Shenoy said, men who are concerned should talk to their doctor about whether they should be screened for prostate cancer. The authors now are surveying prostate cancer specialists in hopes of developing sound guidelines for prostate cancer screening among black men. Authors included Vijayakumar, Shenoy, Dr. Satya Packianathan, a radiation oncologist at UMMC, and Dr. Allen M. Chen, a radiation oncologist at UCLA's David Geffen School of Medicine. 
See the full paper here: http://bmcurol.biomedcentral.com/articles/10.1186/s12894-016-0137-7
|